Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
Providing the best possible end of life care, within the limited resources available, is not a simple task. It requires a dispassionate assessment of the current situation; it demands detailed insight into the local population; and it needs the perspectives of professionals and the people they serve. Good care is founded on the intelligent use of this information.
The Strategy Unit has produced a series of reports that describe the health services that patients use in the last 2 years of their lives. Reports are available for the Midlands region as a whole and for each of the 11 Sustainability and Transformation Partnerships (STP) or Integrated Care Systems in the region.
The reports contain important insights into
- the services that patients use,
- how the patterns of service use change as patients approach death,
- differences in experience by ethnicity, deprivation and cause of death
- the costs of hospital treatment at the end of life and how this varies by STP
- levels of non-beneficial treatments
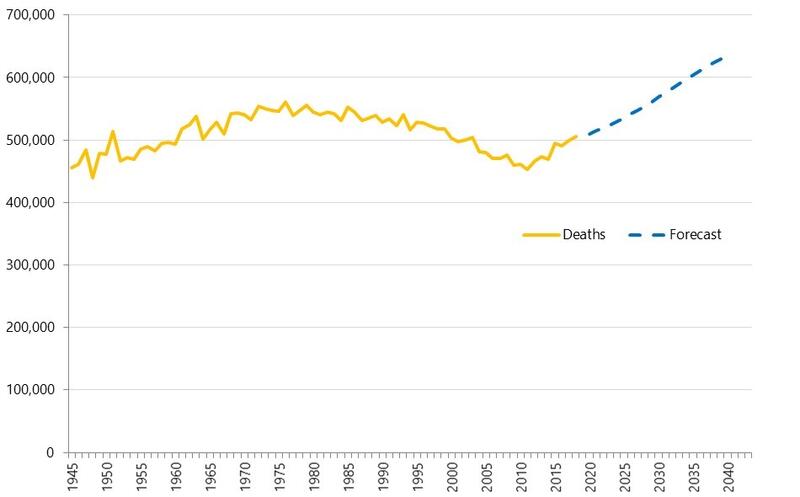
- the additional hospital capacity that may be required to accommodate the projected increase in deaths over the next decade
These reports present a detailed account of ‘what is’. Moving on from this and deciding ‘what ought to be’ is a more complex undertaking. It involves professional judgement, evidence and clinical standards. But it also involves personal preference, values and cultural differences. Combining such diverse perspectives requires care, humanity, and skill.
Seen in this context, the analysis presented here is just one input (albeit an essential one) into a broader set of conversations. These conversations are the place to generate detailed plans for improvement.
Health service use in the last two year of life in...
Report Topic 1 - Background to the Report
Report Topic 1 - Background to the Report
This is the first video of our End of Life series. Lucy Hawkins and Justine Wiltshire discuss the background and details of the report.
Report Topic 2 - People and Place
Report Topic 2 - People and Place
In this video, we delve into the topic of People and Place. We consider who the decedent population are, where they die and what happens on their end of life pathway
Report Topic 3 - Service Use
Report Topic 3 - Service Use
In this video, we look at the topic of utilisation. We consider how much healthcare is used, what types of healthcare are used and how patterns of use vary by proximity to death.
Report Topic 4 - Final Weeks of Life
Report Topic 4 - Final Weeks of Life
In this video, we discuss the final few weeks of life. We consider care close to death, terminal episode length of stay, later chemotherapy and how critical care is used.
End of Life Matters by Peter Spilsbury.
End of Life Matters by Peter Spilsbury.
In this video, our very own Director, Peter Spilsbury, discusses End of Life Matters.
CC BY-NC-ND 4.0

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.