Our previous ground breaking work identified that in England, people with mental health illness have a life expectancy that is on average 16 (women) or 19 (men) years shorter than those without. This difference is thought to be due to poorer access and provision of physical health services for those suffering from a mental health illness.
Starting on World Mental Health Day 2018, the Strategy Unit has been publishing monthly guest blogs to explore different views of the mental and physical health overlap. By gathering these different perspectives we hope to build on the increased awareness from our previous work, bringing more clarity to the specific challenges and to engage others to act for the benefit of those disadvantaged by the overlap.
Professor Sir Muir Gray - Warp and weft – recognising that physical and mental health are interwoven
On World Mental Health Day, we’re delighted to present a guest blog by Professor Sir Muir Gray, the first in a new series of commissioned blogs on the need for new thinking about physical and mental health, building on our ground-breaking work on mental and physical health.
The window of the chapel at Gonville and Caius College in Cambridge has two mathematical symbols that are of great relevance to healthcare. One is the famous table designed by R.A. Fisher that was part of the evolutionary origin of the randomised controlled trial. The other is a Venn diagram, developed by John Venn who was also a master of Gonville and Caius.
Venn diagrams have been used over the years to represent the relationship between disorders of the mind and disorders of the body:
This sharp split between mind and body is misleading. We would be better served by the assumption that all disorders of the body have a “mental” dimension and, conversely that all “mental” disorders have physical consequences too. So, rather than a Venn diagram, we can think in terms of a continuum:
Even this is an over-simplification with the sharp distinction between physical and mental dimensions to health but it is arguably more helpful than the approach represented by the Venn diagram. How we think about the relationship between physical and mental health matters – historically, we have created separate hospitals and services for what have been perceived as two quite distinct classes of patient. As a working principle it is useful, therefore, to base all clinical decision-making on the principles that:
- everyone who has a long-term health problem diagnosed, for example heart failure or rheumatoid arthritis or type 1 diabetes, should be assumed to have, if not ‘mental health problems’, psychological dimensions to the problem that need to be addressed as well as the physical aspects of their problem; and
- everyone with a mental health problem should be assumed to be in need not only of medication and psychological therapy but also activity therapy.
Activity therapy is the new term given to the promotion of activity or exercise for people with long-term health problems. The need for this was emphasised in 2015 in a report of the Academy of Medical Royal Colleges called, dramatically, ‘Exercise the Miracle Cure’. This has been reinforced in 2018 by the launch of the Moving Medicine Programme funded by Sport England and Public Health England, and by the development of the concept of a National Activity Therapy Service by UK Active.
Promoting activity among people with mental health problems reduces the risk of physical health problems such as heart disease. It will, of course, take much more than only the encouragement to exercise to address the severe adverse health problems of people with long-term mental health problems. However, the promotion of activity also, to put it simply, makes people feel better.
What we are seeing now is the recognition that physical and mental wellbeing are interwoven like warp and weft. They cannot be distinguished sharply from one another.
Iain Sinclair’s book called London Orbital records this redoubtable walker’s stroll around the M25, staying as close as he could to that dreadful road. What he encountered on his way around was a significant number of 19th Century asylums, placed in the heartlands of Surrey, Hertfordshire and the other home counties as far as was possible for London County Council to throw them - the same can be seen in many cities. Our challenge now is to unify the services that have been separated for decades.
Professor Sir Muir Gray is a Consultant in Public Health in Oxford University Hospital NHS Trust and a professor in the University of Oxford’s department of Primary Care Health Sciences.
He is also a Consultant in Public Health for www.ukactive.com.
He is the author of Sod70! And with Diana Moran the joint Author of Sod Sitting, Get Moving.
My 25-year career in mental health, has potently revealed to me the dichotomous approaches, interventions and perceptions with regard to physical and mental health. As a house officer in the early 90s, I treated patients with acute and chronic physical health problems and comorbid mental disorders and observed that lack of holistic clinical knowledge and training as well as stigma and fear, negatively impacted on patients’ treatment and prognosis.
A particular young adult with a learning disability comes to mind, an example of where the inability to adequately address the mother’s mental health illness, impacted on the ability of the wider family to cope and care, resulting in the boy being a frequent attender to the inpatient respiratory unit. Spending some time with the mother at the bedside and being interested in understanding how the family managed day to day at home revealed the considerable mental health needs of mother herself and also the broader challenges for the family system. Introduction of psychologically informed home visits to the family, marked a sea change in the family’s resilience and precipitated a significant improvement in this young man’s recovery.
Another noteworthy example is of a 4-year old boy who, under the care of concerned and informed paediatricians, had received months of intrusive investigations for failure to thrive. It took an opportune discussion between a trainee psychiatrist and a paediatrician, that identified that the boy’s caring and compassionate mother had intermittent psychotic episodes, marked by periods during which she would not eat due to fear of being poisoned. The mother’s love and fear for her son’s safety, led to her protecting him from what she saw as potentially dangerous food, resulting in him also harbouring fears of being poisoned. The continued paediatric-psychiatric interactions and the subsequent combined interventions led to recovery for both mother and child and a huge learning for the trainees.
Later in my career, as a forensic adolescent psychiatrist, investigating the poor early life experiences of young people, I regularly identified physical health co-morbidities and soft neurological signs (indicative of neurodevelopmental immaturity due to environmental/social emotional causes). We now have mounting evidence that adverse childhood experiences interfere with epigenetic processes, to the detriment of both physical and mental health.
Mental ill health precipitates, perpetuates, maintains and exacerbates acute and chronic physical health problems.
The challenge for current mental health services is to effectively identify and meet the physical health needs of our patients, so as to alter their current morbidity and mortality rates. To meet that challenge there are number of things we can do as individual clinicians:
Refrain from affirming the false dichotomies – for example in A and E we can train clinical colleagues to overcome the fear, stigma and lack of expertise which manifests as relief when the mental health clinician arrives, alongside comments of “he’s one of yours”.
Be curious, inquisitive and confident to see the patient’s mental health needs beyond the medical/disease process in acute health settings.
Be mindful of each other’s health; we need care and compassion too. A psychiatrist colleague, exposed to years of vicarious emotional trauma through his work, experienced an acute transient ischaemic attack during a particularly challenging psychotherapy session. An oncologist distressed by years of breaking bad news and building relationships with patients while recognising their poor prognosis, shared his distress with his psychiatrist patient while discussing their prognosis. That patient was me!
Of course, it helps to be supported by the wider healthcare system to address the current mental and physical health divide. The most pressing of these considerations to my mind are:
- The development of new integrated models of physical and mental health service provision.
- The training of undergraduate and postgraduate clinicians to deliver these integrated models facilitated by knowledge of systems theory (where the system of interest is interrelated and inter-dependent: physical, biological, psychological, social and cultural, and examines the world in terms of relationships and integration) to raise awareness of the combined effect on physical and mental health.
- The adoption of comprehensive approaches to meet mental and physical health care needs, not just for our service users but also for our clinicians.
Jennifer Dixon, Chief Executive of the Health Foundation, reflects on the relationship between mental and physical health and the need for better integration of care.
The past five years have seen much discussion about the effect of societal changes on the health of the population in the UK. This has been prompted by a stalling growth in healthy life expectancy since 2010 and a growing gap in levels of health and disability between the most and least deprived populations. For example, one recent study showed that age-standardised rates of years of life lost were twice as high in Blackpool as in Wokingham(1).
The long list of structural changes commonly discussed include the wider determinants of health. In particular: the impact on the economy of austerity following 2008; the changing nature of work (stagnating wage growth, loss of traditional blue-collar employment and growth of highly insecure jobs); the widespread use of social media; family breakdown; inequalities in wealth, and demographic change.
The increase in mental health conditions
Given such stressors, it is perhaps not surprising that mental health conditions appear to be increasing in the UK population, particularly in deprived populations and women. There are two waves. The first is in young people, where prevalence has slightly increased over the past 20 years – a pattern also seen internationally. Young women have higher and increasing rates of common mental disorders and self-harm, and since 2007 the gap between genders has increased. The second is in older people, especially those over 70 years of age, who are increasingly living with various forms of age-related cognitive impairment, including dementia. The rising prevalence is mainly due to increased numbers of older people in the population.
The best estimates of the proportion of adults (aged 16 and over) having a mental or emotional problem in England come from the Adult Psychiatric Morbidity Survey (2)
- One in six (17%) adults 16 years or older met the criteria for a common mental disorder (such as anxiety or depression) in 2014, an increase since 2000 mainly in women.
- 39% of adults aged 16–74 years with a common mental disorder were accessing mental health treatment in 2014 – up from 24% in 2007.
For the young, the best estimates come from the Mental Health of Children and Young People in England, 2017 (3):
- One in eight (12.8%) 5- to 19-year-olds had at least one mental disorder - a rate slightly increasing over the past 20 years. The highest rise in prevalence was in women aged 17–19 years (now nearly one in four, or 23.9%).
- Emotional disorders were the most prevalent type in 5- to 19-year-olds (8.1%) and are the main group to have risen since 1999.
- The prevalence of disorders increases with age: 5.5% of 2- to 4-year-olds compared with 16.9% of 17- to 19-year-olds.
- 28.5% of children and young people aged 5–19 years were reported to have had contact with professional services (20.9%) or informal support (18.2%); 4.5% of children had had contact with a mental health specialist.
Use of NHS-funded health care
Identifying the extent to which people with a mental health condition use NHS-funded health care or other public services is far from straightforward. Many people are cared for in the community by general practice or other providers. The routinely collected data are either of poor quality, not accessible, or difficult to link up to show a complete picture of the care received by individuals. It is also difficult to link data on the use of other public services by people with mental health conditions to NHS data.
NHS Digital provides the most detailed picture of the NHS-funded health care received by people who used secondary mental health services in England. However, the data on the use of this care are grouped together for people who have a mental disorder, learning disability or autism. In 2017/18, 4–5% of the population had contact with such NHS-funded care for these conditions. There is a bulge at 16 years (12% women, 9% men) and 17 years (11% women, 8% men) were in contact with services, then a decline, and then a steep rise for people 80–89 years (women 12%, men 11%) and 90 years and older (women 18%, men 16%). It isn’t clear yet if the ‘teen bulge’ will be carried forward as the cohort ages.
The link between mental and physical health
It has been known for some time that people with a mental health condition are more likely to have a physical illness and die earlier. The Strategy Unit’s fascinating analysis linked NHS hospital episode statistics data on the use of NHS-funded care in NHS Trusts for individuals with ONS data from death certificates, and compared the mortality of those with recorded mental health problems to those without (4). Life expectancy at birth for people who became mental health service users was calculated to be a staggering 19.1 years shorter for men with a mental health condition and 16.1 years shorter for women, relative to those without. This is roughly double the gap in life expectancy between the most- and least-deprived populations in England. The shortest life expectancy for mental health users was in populations living in Cornwall and in the north east and north west of England.
Between 2006 and 2015, the sustainability and transformation partnership (STP) areas with the biggest drops in life expectancy for mental health service users were Durham, Darlington and Tees and several STPs in the Midlands. Conditions causing death that were more common in mental health service users included ‘external causes’ (such as injury, poisoning, suicide), cancer and circulatory, respiratory and digestive disorders. In other words, people with a mental health condition often have other significant conditions too – a fact known for some time. In his Harveian Oration in 2016, Chris Whitty noted that people with multiple conditions had ‘non-random series of predictable disease clusters’. The single most common condition in a cluster is depression.
According to the Strategy Unit’s model, a young person with a first episode of psychosis, but initially physically well, is more likely to gain weight, smoke, abuse substances and live unhealthily, increasing their risk of a range of illnesses at a relatively early age. Unsurprisingly, people with mental health conditions use more health care relative to people without. A&E attendance and unplanned hospitalisation rates are 2–3 times higher (especially for people with personality disorders) and use of diagnostic services twice as high. There is much less difference for planned care.
Improving the integration of mental and physical health care
These figures say nothing about the quality of care received or access to care, which we know need to improve significantly, or do more than hint at opportunities for prevention. The close relationship between mental and physical ill health has led for many to call for the NHS to integrate care around the person, rather than treatment in specialist silos, and to pay far more attention to risk factors and preventive health care. As Whitty noted in his Oration, ‘as a generation we have been more effective at tackling the biological rather than behavioural drivers of disease’. This orientation is reflected in the volume and nature of scientific inquiry into disease, as well as the approach to treatment.
The Strategy Unit usefully sets out what STPs can do in practice to address mental and physical health together. The progress made in the last 5 years in dementia care shows that it can be done. Hopes are high for the forthcoming NHS 10-year plan and, assuming integrated care is still being pursued with vigour, new service models treating mind and body together must surely be a priority.
Several areas of the country are pioneering this type of care, for example as part of NHS England’s Improving Access to Psychological Therapies and Improving Physical Healthcare for Serious Mental Illness programmes, and careful evaluation will be important. This isn’t just an issue of parity of esteem, important though that is, but one of comprehending the nature of ill health and wellbeing to be more effective in reducing mounting risks in the future.
Jennifer Dixon (@JenniferTHF) is Chief Executive at the Health Foundation
References
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)3220…
- https://digital.nhs.uk/data-and-information/publications/statistical/adult-psychiatric-morbidity-survey/adult-psychiatric-morbidity-survey-survey-of-mental-health-and-wellbeing-england-2014
- https://digital.nhs.uk/data-and-information/publications/statistical/me…
- https://www.strategyunitwm.nhs.uk/publications/making-case-integrating-…
Sophie Corlett the Director of External Relations at Mind provides some perspectives from people with physical ailments who are users of mental health services.
Mind’s work is driven by people’s experiences and last year, we spoke to people across England and Wales about the care they received for their physical and mental health. One of the top issues they raised was that they wanted services that listened to them and believed them. We hear over and over from people[i] with mental health problems that they have struggled to have their physical health conditions taken seriously and not dismissed as a symptom of their mental health problem, leading to delayed care and sometimes tragic outcomes.
When I was in Cumbria I knew there was something wrong with my heart, I was getting funny pains, I was having funny dos and I didn’t know what on earth was going on. I just felt awful. I kept going to the doctors and saying, “There’s something wrong with my heart.” And he’d say, “Well how do you know?” It took me ages, a long time to say, “I need to see a heart specialist.” And I just got to see one up in Cumbria but then I moved so I had to go through the process again when I came down here and they were like, “Why do you want to see a heart specialist?” I said, “There’s something wrong with my heart, I know there is, I keep having these awful dos, I’ve never had them in my life, they’re nothing to do with my fibromyalgia or anything else, please believe me, I know there’s something wrong.” But the doctor just kept umming and ahhing, putting it off. Then last year when I was really, really poorly, I finally got the results of my scan back and I’ve got a hole in my heart and I need an operation. I had to say so many times how poorly I was and that there was something wrong with my heart because they didn’t believe me. But I just knew there was. I said, “I want to see a specialist, I want to know what’s wrong with it. I know there’s something not right.” It’s horrible when you have to be like that with your doctor. It’s upsetting. And you feel like it’s just because they know you’ve got mental health, that they don’t believe you. - David’s story.
Many of us will be familiar with the statistics: people with physical long-term conditions are two-to-three times more likely to experience mental health problems than the general population. We also know that people with severe mental illness die on average 15 to 20 years earlier, mainly due to physical health problems. Our mental and physical health are interdependent, and yet at Mind, we often hear from people who feel an unhelpful, even harmful, distinction made between their physical health and mental health.
We’ve been to some appointments where they’ve specifically said, “You can only come about one thing.” So if you come in and you say, “My pain is making my mental health worse.” They’ll say, “Let’s make another appointment to come back." - Ray
People want integrated services that treat the whole person. Again and again, we heard how people are forced to navigate a maze of services which treat one aspect of their health, which don’t communicate with each other, and fail to see the person behind the condition.
Gone are the days when everything was all under one roof – you knew where you were – nowadays you just bounce over multi-agencies, like a grenade with a pin removed, so I don’t know what the hell’s going on; I’m damn sure anybody else here doesn’t know what’s going on, because there’s no central point. - Sam
And finally, people wanted aspirational, goal-based care that is based on their own goals. They wanted clinicians to be more creative in their approaches, for example, using social prescribing to achieve goals for physical and mental wellbeing together or to tackle loneliness.
Well mine is loneliness. I’ve got nobody ... I go days without seeing anyone. I do a bit of volunteering and I do a bit of shopping that’s all and I’ve got my 3 stray cats. I can go days without seeing anyone. It seems everybody’s got somebody. I am lonely. - Chris
None of this is easy to achieve. Systems will need to work together to provide wrap-around support for people with complex conditions. It takes time and perseverance to build the sorts of relationships and trust required for services to give away autonomy, pool budgets or share plans, in pursuit of better patient outcomes in the longer term. But though this is slow work, where we have seen greater collaboration, people’s experiences of care have improved hugely.
And alongside changes to systems, we need to equip and support those at the front line of caring for our health. For example, GPs tell us that they want access to, and time for, more mental health training to build their confidence and similarly, specialist mental health staff can feel outside their comfort zone when dealing with physical health conditions on inpatient wards. And we need to relieve the unsustainable workforce pressures on those providing care so that they have the right support when they are struggling without fearing the consequences.
We know change is possible because we have seen it in pockets around the country. We want to see these exceptions become the norm, so that caring, confident, holistic treatment is available for all of us, wherever we live.
[i] All names below have been changed to provide anonymity.
Dr Paul Turner, General Practitioner at Karis Medical Centre, Birmingham and Joint Clinical Director for Mental Health, NHSE West Midlands Clinical Network describes the cost of untreated complexity.
In the first blog of this series Professor Sir Muir Gray succinctly describes the interdependency between mind and body as “warp and weft”; like indivisible fibres of fabric and challenges us to unify the services that have been separated for decades.
Much earlier, Julian Tudor Hart wrote “The availability of good medical care tends to vary inversely with the need for it in the population served. This inverse care law operates more completely where medical care is most exposed to market forces…” (1)
Whilst the context and times in which he wrote were different, the central message still rings true: there exists a “forgotten majority” of people with complex mental distress, often trauma-related, for whom our silos of thinking and care allow gaping holes in and between medical and social services to persist.
Without undermining the considerable investment and advances in the care of people with mental health problems in this country, people experiencing distress continue to fall through gaps on a daily basis. Almost as though our services are patches in a quilt which have not been sewn together. In order that, together, we can make collaborative and creative changes which unify our approach to these people, it is vital that we know the true extent of their need.
In short, we need to start counting complexity
Whilst human expressions of suffering do not distinguish between mind and body - we manifest our distress in the manner which circumstances allow - most of our services continue to do so unflinchingly. One consequence of this is that we undervalue listening and understanding what has happened to a person as we focus on what is “wrong’ with them. This disproportionately affects the people who don’t fit into our paradigm of intervention- based services, and yet who often suffer the most.
Here are some of the consequences of such gaps:
- One out of every 2 people referred by their GP to a new outpatient appointment with persistent physical symptoms, will not be found to have a physical cause for their problem. (2)
- 2/3rds of people who present in mental distress do not find their needs being met. (3)
- 70% of people who take their own lives have seen their GP in the previous year but only 8% were referred to specialist mental health services. (4)
- Antidepressant prescribing has doubled in the last 10 years (mainly long-term prescribing). (5)
- Chronic pain prescribing (particularly gabapentinoids and opioids) continues to escalate, whilst recognition of the near-universal impact of underlying adverse childhood experiences in this group is scant (See Dr Paul Roberts blog in this series).
Just sit back and think for a moment or two about these anomalies in our health care. Bold and brave as the Five Year Forward View for mental health was, it was not designed to answer these questions. Existing funded provision for helping people manage their distress is mainly focussed through local interpretations of the Improving Access to Psychological Services (IAPT) programme and specialist mental health services. However only about one in four people referred to IAPT will recover and the large majority of people referred to specialist mental health services are not offered a service.
Just as IAPT does not purport to solve all psychological problems, neither should we expect specialist mental health care to manage all complexity. Another approach is needed - But what else is there? It is not enough to hope that people will be “signposted to the Third Sector”. Neither is it reasonable that large numbers of people continue to present in mental distress to A&E, whilst Police, Ambulance and Fire Service staff are increasingly involved in supporting people with complex care needs because health services can’t cope.
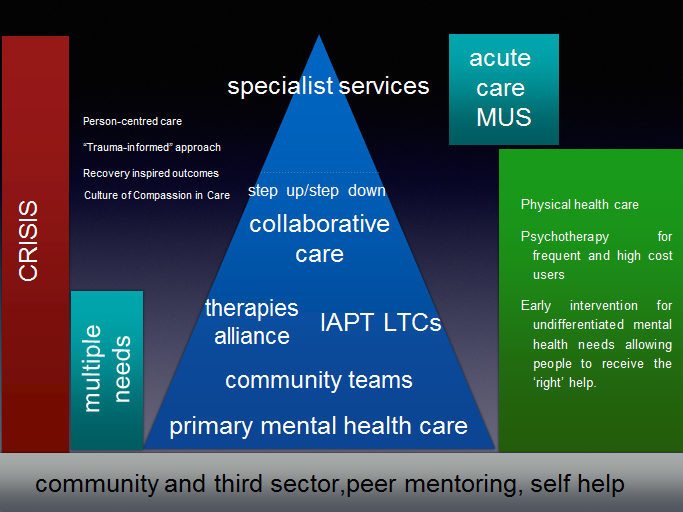
The NHS Long Term Plan paves the way for considerable re-imagining, embedding and sustaining primary mental health care with the development of collaborative primary care based services, but in order to really ensure that people don’t continue to fall through gaps in care and support, we need to be able to define more clearly who these people are rather than only stocktaking our successes.
The considerable evidence of the benefit of collaborative care in Mental Health, extensively research by Professor Linda Gask and others, has been overlooked as we favour a competitive target-driven approach to flourish (6). Commissioning for collaboration may require us to develop new approaches.
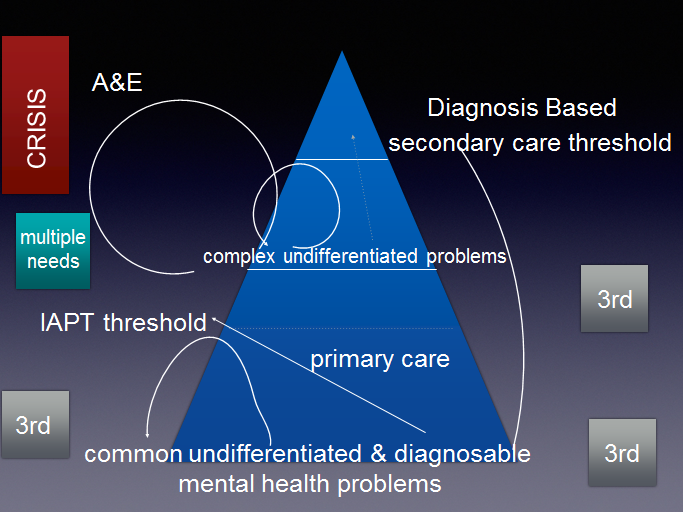
Unsupported, or inadequately supported, people are often given treatment or undergo repeated investigations that do not help, leaving them, their families and their clinicians feeling disappointed, powerless and stressed. The figure below illustrates what happens when people with a range of undifferentiated problems don’t meet threshold for care.
Thresholds are perfectly reasonable, it is equally reasonable to appreciate what they mean for complex human beings.
Figure 1 illustrates how people who don’t meet service thresholds in a disjointed system can fall through gaps, circling in and out of care which is not designed to meet their need. (3rd refers to voluntary & charitable sector organisations; MUS refers to medically unexplained (or persistent physical) symptoms.)
Figure 2 suggests how this could be different in a collaborative system where the complex psychosocial factors in peoples’ lives are recognised and addressed more effectively.
Sharing problems, solutions and successes is the essence of effective community, coupled with the collective accountability to identify them. Our framing of the scale of the task is thwarted by only counting (and thus being accountable for) the people we think we can provide interventions for. The complex human distress confronted by Patients, families and frontline clinicians doesn’t afford us such luxury.
The West Midlands Strategy Unit are currently in the process of collating regional data to attempt to define those people affected by gaps in mental health provision. How differently could we provide patient and family centred care in integrated care systems if we collectively also counted those whom we currently cannot offer an adequate service?
In one of his earliest speeches as chief executive of NHS England (7); Simon Stevens said:
“together we’re going to need to work in coherent and purposeful partnership, because the national leadership of the NHS has to be more than the sum of its parts.
The alternative, to quote Milton’s Paradise Lost: ‘Thus they in mutual accusation spent/The fruitless hours…And of their vain contest appeared no end.’ Given everything facing us, we don’t have fruitless hours to waste, and we can’t afford vain contests. Said less poetically, it’s time to roll up our sleeves, pull together, and get on with it.
The health care system that can solve-for the really big challenges – dementia, obesity, inequalities, mental health and wellbeing, personalisation, prevention and empowerment – that’s the health system that will prosper in the 21st century.”
Examples of creative joint working using all the skills and tools at our disposal abound, but they are still at the margins of health policy and commissioning. Insanity, as Albert Einstein famously intoned, is “doing the same thing in the same way and expecting different results”.
Now there’s a diagnosis which really needs treatment.
[2] Bermingham. 4 Bermingham, S.L., Cohen, A., Hague, J., & Parsonage, M. (2010) The cost of somatisation among the working-age population in England for the year 2008- 2009. Mental Health in Family Medicine, 7(2): pp71-84.
[3] Adult Psychiatric Morbidity Survey: Mental Health and Wellbeing, England, 2014. Available at: https://www.gov.uk/government/statistics/adult-psychiatric-morbidity-survey-mental-health-and-wellbeing-england-2014
[4] Suicide in primary care in England: 2002-2011. National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (NCISH). Manchester: University of Manchester 2014.
[5] https://digital.nhs.uk/news-and-events/news-archive/2017-news-archive/antidepressants-were-the-area-with-largest-increase-in-prescription-items-in-2016 accessed 26/2/2019
[6] Gask L How can we work more effectively across the interface between psychiatry and primary care? Systematic Review 2017
The relationship between diabetes and mental health is complex and significant. In 2017, we consulted with over 9,000 people living with or affected by with diabetes, a broad and far-reaching piece of work which resulted in our Future of Diabetes Report.
Through this consultation, we found that 63% of people often or sometimes feel down because of diabetes, with parents of children with Type 1 most likely to be affected. One respondent told us:
“The worst thing is the sheer isolation, I’m left to work it all out on my own with no help or support.”
A third told us they would be keen to have support from a trained professional:
“It’s hard for friends and family to really understand and they misinterpret your mood.”
People with diabetes experience disproportionately high rates of mental health problems such as depression, anxiety and eating disorders. Living with diabetes is a ‘mind game’. The prospect of complications, and for many (e.g. those with Type 1 diabetes, those with Type 2 on variable insulin doses, and those with complications), the constant hour-by-hour management of the condition make it an incredible emotional burden.
People living with diabetes tell us that the biggest issue is that they don’t feel their emotional health is looked after. They tell us that healthcare professionals can be preoccupied with numbers, and reducing the risk of physical complications – stroke, amputation, blindness – while avoiding the issue of mental or emotional health. They also tell us they don’t think their diabetes team can help, and that they feel ashamed for not coping.
But second to this, and perhaps more insidiously, people with diabetes of whatever type, are the target of widespread stigma. This stigma has two main elements: There are strong widely held beliefs that people with Type 2 diabetes have no one to blame but themselves for having diabetes, and that their lifestyle choices have led to the condition; ‘fat’, ‘lazy’, ‘brought it on himself’, are the kinder phrases.
In our services we know that people with Type 2 diabetes will rarely be involved in social media networks. They get too much of a hammering if they out themselves as having Type 2 diabetes. Instead they tend to contact us anonymously through our Online Forum. Conversely, this stigma reaches across to those with Type 1 diabetes, who have to constantly remind people that theirs is an autoimmune condition.
The other strong source of stigma is the pressure to meet the ‘ideal’ of good diabetes management. Management of diabetes can therefore become a numbers game; there’s so much data – blood glucose, HbA1c, blood pressure – surrounding management of diabetes, and people with diabetes have a vision for what ‘good control’ of diabetes looks like, so failure if they fall short of what they feel amounts to good, ‘ideal’ control, they can feel like a failure.
So why is poor mental health an issue? Simply put, the issue is that poor emotional health can affect diabetes management, and in turn the daily grind of diabetes management can affect emotional health.
The Diabetes UK report Minding the Gap (2008) showed that 85% of people with diabetes in the UK have either no defined access to psychological support and care, or only local generic services where knowledge of diabetes may be very limited. Our experience tells us that not much has changed in that respect. The report of the Diabetes All Party Parliamentary Group last year (2018) found that diabetes consultations provide limited opportunities to talk about emotional wellbeing; that national policy focus does not fully cater for all levels of need; that some access to psychological support in diabetes teams is patchy ; and that there are widespread challenges in rising demand allied to financial pressures – meaning waiting times for specialist services (including those for children and young people) were high.
Yet, the APPG report also found excellent practice and support in place in some areas. While this is a problem that’s been around for a long time, I have hope that now, as the health system moves to bridge the divide between physical and mental health, and as a society we are talking about mental health issues the time is right to find solutions.
What can we change? Well, small changes can make a big difference. One gentleman said to us:
“I would like to be asked “how are you”? Not how is your diabetes? How are your sugars? How’s your sight, feet, kidney function… I am not a computer screen of test results, and even a nod to that would improve matters so much for me.”
Assessment and support for mental health issues should be a routine part of diabetes care. There are great examples of best practice, which shows that it can be done. Increased training of diabetes healthcare professionals in mental health can help them recognise symptoms and provide support themselves. Dedicated time from a mental health professional to a diabetes service, can help to advise the team and provide care and treatment themselves if necessary for cases that require psychological/psychiatric input. We need to ensure that this is consistently provided everywhere and that everyone with diabetes has access to appropriate support for their mental health when they need it.
A broader understanding of the benefits of integrating physical and mental health will mean that there is more support across the NHS for setting up these services. Support is not always expensive. More options for peer support, mentoring both online and face to face can make a big difference. There is more research needed on diabetes and mental health, which has been highlighted by the Clinical Studies Groups we have been supporting.
We at Diabetes UK can help too. We have recently launched the ‘Diabetes and emotional health’ guide to help healthcare professionals to support the emotional needs of adults with diabetes. We will also be running an emotional health ChangeLab where healthcare professionals, people living with diabetes and their families and carers will look at ways to make emotional wellbeing a routine part of diabetes care.
We can also offer support to people with the condition. We have a Helpline, an online community Forum who give wise and sage advice, and we also have 360 local groups who can provide peer support and a sense of community. Our Helpline number is 0345 123 2399 and you can find out more about the support we offer on our website www.diabetes.org.uk
Dr Paul Roberts, Director of the North Staffordshire GP Federation provides a GP perspective in his contribution to the Strategy Unit’s guest blog series which explores the mental health and physical health divide. He focuses on the painful conversations between the patient and GP which are rooted in health inequalities.
Painful conversations. A GP perspective on chronic pain.
It doesn’t happen very often, but it is recognisable to anyone working within primary care in an urban, deprived environment. The rise of a voice from a room in the corridor, the pulse quickening for everyone hearing, and then the inevitable slammed door. Sometimes the shouting continues in the corridor, falling away as the disgruntled individual and their entourage leave. The collectively held breath is released; today we don’t have to intervene. A quick screen message is sent to the clinician: R U OK? There is a response of J, of course they aren’t really but we all have to pretend…
It is easy to see such dysfunctional consultations in terms of being someone’s fault. The reality is that there is often a lifelong trajectory behind the moment of that slammed door. For a clinician, the inevitable conflict can be anticipated, but seldom averted.
The roots typically arise from the mix of nature, nurture and environment impacting on an individual in their early forties, without specific skills and unable to compete for the shrinking number of manual roles they were previously undertaking. Such individuals drift out of the job market, becoming more stressed as the real-world pressures mount. They are no longer as fast or agile, they have musculoskeletal pain and want it fixing. For a while their acute pain can be managed by increasing acute analgesia, but for some a symptom such as a mechanical low back pain doesn’t go away. There follows a descent into increasing immobility, deconditioning and increasing pain, augmented by increasingly poor mental wellbeing that comes to a head when the benefits agency assesses them as fit for some work. Austerity Britain has not helped, neither has the unfair stigma of ‘scrounger’ for those who find themselves in this position.
As GPs observing a bad situation getting worse, we want to help. This individual will have had their physio intervention and likely the MRI which demonstrates no target for an operation. The codeine they had been given quickly stopped working so at some point they were offered something akin to morphine. The moment of crisis was averted for that moment.
The reality is far more complicated: the person is hurting, emotionally, physically and possibly existentially but is most likely to experience, and describe, this complexity of emotion in terms of a physical pain.
At the time of the critical consultation, the patient is starting to get side effects from the medication we are offering but is still in pain and asking for more pain relief. The honest conversation that happens next is really tough. Neuroscience is only just beginning to unpick the pathology of how chronic pain develops as a central emotional response to a group of circumstances rather than as a specific response to physical tissue damage. We are often left floundering with explanations; even when one starts by affirming that the pain that is experienced is real, the message heard is the ‘pain is in your head’. The sense of anger that this engenders is not assuaged by the polite refusal to increase the dose of the prescribed pain killers. Emotion denies the possibility of shared understanding and the common result is that the patient leaves, angry, not having had their needs met. A painful consultation from everyone’s perspective.
What could be different?
Learn and share our experience. There is a need for a cultural change in the collective belief in the magic of western physical medicine to cure people, whatever their problem and often within the 10-12 minute appointment in general practice! Current practice is slowly changing but there are many individuals who are at risk from being treated with opiates for chronic pain. We know now that this is doing little good and almost certainly some harm. The Royal College of Anaesthetists have produced sensible accessible guidance.
Continue to care with compassion, but through a different lens. There are undoubtedly situations in which surgical intervention is positively lifechanging and there are others where it might be. We need to follow the evidence, where it exists, but avoid the collusion of referring and intervening in other circumstances outside well designed trials. Referrals in these latter situations might solve the immediate problem of concluding a consultation within 10 minutes, but increase the likelihood of a future painful conversation.
Chronic pain is too common to be left to specialists. The standard NHS response is to commission a specialist service, which is usually costly, generates low activity, long waiting times and often disappointing outcomes. My assertion is that the most important single factor in supporting a patient with a chronic pain and their family to make progress is an enduring positive relationship with a clinician. General practitioners are ideally placed to do this, but the current contracting milieu makes this incredibly difficult. Funding has shifted away from primary care, a shift back towards providing one whole time GP equivalent to less than 1500 individuals would create a space to make this possible. Chronic pain specialism needs to be embedded as a population health resource as well as in specialist secondary care clinics. Low intensity community psychological services, community occupational therapy and physiotherapy services also need to be aligned with the goal of improving the function of those identified as having chronic pain.
Chronic pain is another manifestation of health inequality. We have started to recognise that many social and environmental elements converge to make chronic pain yet another health inequality with many of the same determinants as others. As a society we need to create more opportunities for those who do not cope well in school to acquire a wider repertoire of life and learning skills, so they can be more individually resilient. We should see chronic pain as a condition that requires primary, secondary and tertiary prevention strategies and include it in our system strategic thinking.
Dr Paul Roberts, Director of the North Staffordshire GP Federation