Waiting lists for elective care are in the news. The national plan has been issued, with the expectation that lists will continue to rise for some years - and that long waiting will not disappear anytime soon. Addressing this ‘backlog’ will remain a fundamental challenge for some time to come.
This raises the question of how people on the lists are prioritised. There are millions of people waiting for treatment. How should we decide who gets called first?
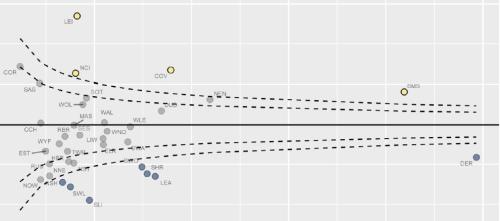
Previous Strategy Unit work showed that there is already inequity: richer people tend to get better access to elective treatment than poorer people. This trend emerged over the last decade. And, if we aren’t very careful, the final reckoning of how the NHS ‘recovers’ will see these inequities made much worse.
Who gets treated ahead of whom is a value judgement. No one has a monopoly on those – and there are no right or wrong answers.
To date, the NHS has largely worked by prioritising based on length of wait. During lockdown the NHS/government worked with the Royal Colleges to establish a clinical priority weighting system. So decisions about who to treat started by considering clinical priority, then length of wait.
This seems utterly reasonable, but is it sufficient?
Let me explain why it might not be.
Imagine that two people are waiting for a procedure that has a non-urgent clinical priority. In both cases, they have pain that seriously limits their mobility. The first, Patient A, has waited for 50 weeks. The second, Patient B, has waited for 20 weeks. A slot is available for the treatment they both need. Who gets called?
Based on the information you have at this stage, who would you choose?
Now let me add some more information. Patient A lives in an area that is in the upper quartile of socioeconomic status; Patient B lives in an area from the lower quartile. People living in upper quartile areas typically get greater access to this treatment (relative to need) than people living in the lower quartile.
Would that change your judgement?
Now some more information. Patient A is otherwise well and has a job that allows them to work from home at a desk. Patient B works on a building site, on a zero hours contract, and has underlying mental health issues.
Would that change your judgement?
These are complex considerations. And they are value judgements, so they entail difficult debates where final positions are hard to justify using evidence. So many of us might want to avoid this discussion, treating ‘clinical priority’ as though it were a single, neutral and over-ridding consideration.
But this is an illusion. Carrying on just doing what we’ve always done is as much a value-based position as changing it. There is no ‘neutral’ position. Choosing purely on time waited is a deliberate decision to NOT take into account other issues. So we MUST engage in the question.
And that is why I’m really excited that the Strategy Unit is helping to inform these debates. We are starting with two exciting pieces of work.
The first is with our colleagues at University Hospitals Coventry and Warwickshire NHS Trust. They have developed a waiting list prioritisation system that starts to incorporate socio-economic factors into their approach to working through waiting lists.
They have asked the Strategy Unit and our partners Ipsos MORI to work with them in exploring with their local populations what they think about these issues. This is a vital step as a key challenge to formalising value judgements in prioritisation decisions is about how to secure some form of legitimacy. The project involves running properly designed deliberative events and surveys with people in Coventry and Warwickshire to explore how they think about trade- offs in terms of individual prioritisation. What do they think matters when it comes to making these decisions?
It will then be for the decision makers in that patch, having heard that, to decide how they will prioritise. And they will do that with explicit reference to what they’ve heard from their public. We will then be working with the Trust to evaluate whether the approach they settle upon helps to achieve their objectives.
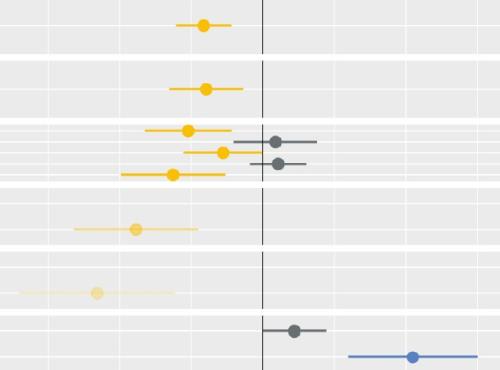
The second piece of work is more analytical. Following on from our work that showed current inequity, we will shortly publish a report that reviews the various strategies that can be adopted to tackle socioeconomic inequity in planned care. You can find out more about this work, which we are doing for the Midlands Decision Support Network, here.
Both pieces of work are a starting point for us. The scale and importance of the challenge means that the Strategy Unit will want to continue to apply our skills and efforts. And the nature of the questions involved in this topic means that multiple approaches, viewpoints and efforts are needed.
Collaboration is essential. So we would like to hear from other organisations as they approach waiting lists and the question of ‘what is fair?’