Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
So how can local Integrated Care Systems (ICSs) go about changing this? Tackling health inequalities is one of the four aims set for ICSs, so where should they start?
The first step must be gaining a clear-eyed sense of the problem. This requires analysis to highlight inequalities that could be addressed. The next step must be to apply explicit criteria to focus decision makers’ attention.
The analysis below, produced for Black Country and West Birmingham, addresses these needs. We are sharing it here because we think other ICSs may benefit from having this for their system.
The analysis:
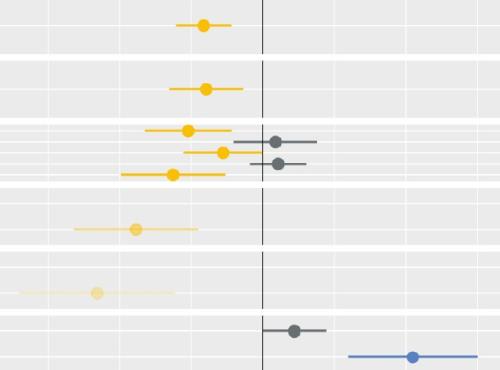
It covers 21 clinical areas and looks at inequalities across ethnic and socioeconomic groups. But it does so using a single outcome measure: emergency hospital admission rates. This outcome is distressing for individuals; expensive for systems; and indicative of broader problems. It simplifies inherent complexity.
We show both the scale (numbers affected) and the degree (the relative unevenness of admission rates across subgroups) of the problem. Applying these criteria cuts through the noise often generated by the proliferation of ever-fuller data sets. It shows Black Country and West Birmingham where the gains are.
We find that people from specific ethnic minority groups are far more likely to be discharged from hospital without a firm diagnosis coded in their record. There are many possible explanations, but we have ruled out data quality. This requires attention: ICSs cannot address what they cannot see.
Please contact us (strategy.unit@nhs.net) if you would like us to replicate this analysis for your ICS.
CC BY-NC-ND 4.0

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.