
10-Year Productivity Forecast for the English NHS: An Expert Elicitation Study
Expert elicitation exercise commissioned by and in collaboration with the Health Foundation has produced forecasts of NHS productivity rates over the next 10 years.
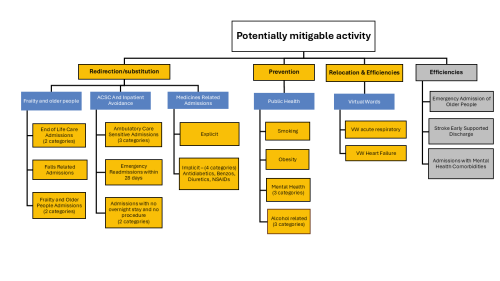
Shifting care ‘from hospital to community’: where to start?
What are the opportunities to shift activity from hospital to community? Our analysis provides an evidence-based place to start.

Expectations: The hidden driver of healthcare demand
How well do we understand changing expectations and implications for the NHS?

A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.
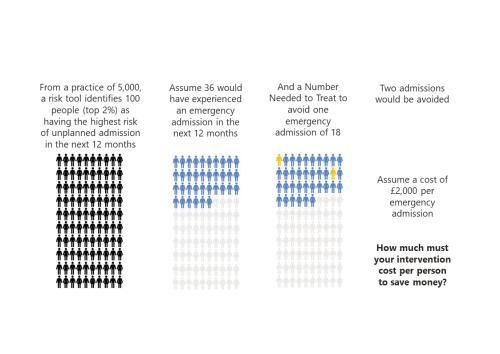
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.

A Picture of End-of-Life Care in England
Working with Macmillan our analysis investigates who is more likely to experience poor outcomes associated with shortcomings in end-of-life care? Are there particular areas in England where those at end-of-life face significant challenges and how might the supply of services in an area be influencing these?
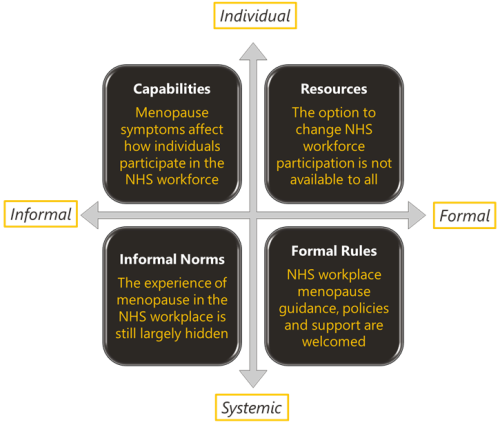
Menopause and the NHS workforce
The impact of the menopause on the NHS workforce. The Strategy Unit and Health Economics Unit report on their mixed methods findings.

What’s philosophy got to do with evidence reviews?
Ever wondered how to make better use of evidence in decision-making? Follow our latest blog series to find out more about how our Evidence and Knowledge Mobilisation team can help you to make sense of and use evidence from research and practice.

Could a peer review methodology help drive continual learning within and across local systems?
In this blog Karen describes how peer review methodologies are being used to support learning in Long COVID services.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).

Advancing the analytical capability of the NHS and its ICS partners
The Strategy Unit were asked by the Strategy and Development Team in the Directorate of the Chief Data and Analytics Officer, NHSE/I, to make recommendations for advancing analytical capability across the health and care workforce.
INSIGHT 2021: Data for the head, stories for the heart
Death is certain, yet our planning doesn’t reflect this.
INSIGHT 2021: Data for the head, stories for the heart
Death is certain, yet our planning doesn’t reflect this.
INSIGHT 2021: Insight to Action. What Works?
It has been estimated that it can take up to 17 years to translate evidence into practice – how can we change that?

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department

Learning the lessons of Long Covid in real time
Round table event, 12 July

How can analysis help clinicians improve services? Interview with Dr Anna Lock
Dr Anna Lock, Justine Wiltshire and Lucy Hawkins reflect on the Strategy Unit's innovative end of life care analysis. How can this work help clinicians to improve services?

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
Evaluating Artificial Intelligence: a significant new win
The Strategy Unit, the Health Economics Unit and Leicester Clinical Trials Unit have been announced as evaluation partners to support success in the Artificial Intelligence (AI) in Health and Care Awards.

Making sense of evidence
It's time to celebrate World Evidence-Based Healthcare (EBHC) Day. In a world dominated by COVID-19 and the associated infodemic, this day arguably has more resonance. Closer to home, EBHC Day also coincides with our Insight 2020 festival and the launch of the Midlands Decision Support network. What better opportunity to ask, 'what does evidence-informed decision making actually mean'?