World Menopause Day 2023 update
On World Menopause Day 2023, we’re pleased to share our in-depth quantitative and qualitative reports. These provide more detailed findings, underpinning the overarching triangulated report published last year. The qualitative report includes case studies illustrating the experiences of staff identifying as menopausal from six participating NHS organisations. We hope these detailed and overarching reports, provide the impetus for change for the benefit of the workforce in both the NHS and beyond.
One in five NHS workers is of menopausal age, yet until recently little has been discussed about the effect this has on their health and wellbeing. Last week NHS England Chief Executive Amanda Pritchard launched new guidance aimed at supporting NHS workers through menopause. But what are the stories behind these headlines? Our new report, published today, takes a unique in-depth approach to examining the impact of menopause on the NHS, combining data analysis and in-person interviews to give the most comprehensive picture yet.
The Strategy Unit and the Health Economics Unit worked together to use their specialist expertise in research, analysis, and economic modelling to explore the hidden issue of the menopause in the workplace.
Menopause is a life stage for women; for most, it’s a biological transition as menstruation ceases. In the UK, the average age for a woman to reach menopause is 51, but this can range from 45 to 55 years of age. The experience of menopause is not uniform, and women seek support and treatment differently. There is also a difference in the care and treatment received, even from clinicians, when women seek help for their menopausal symptoms.
Given the NHS is the biggest employer in Europe, predominantly of women, the study focused on this large workforce of women (over one million or 76% of the total NHS workforce) who are of menopausal age (over 260000 or 19% of the total NHS workforce).
Using a mixed methods (qualitative, quantitative, and economic) analytical approach the study asked:
- What are the characteristics of the NHS employees assumed to have menopausal symptoms?
- What is it like to experience the menopause as an NHS employee?
- What does the menopause cost the NHS as an employer?
A range of symptoms associated with the menopause were reported by participants of the qualitative (interview) study. Cognitive symptoms such as brain fog and memory loss were commonly described by the participants as affecting their ability to work. Many stated a crisis of confidence in their roles, and described instances of being overwhelmed, ‘imposters’ and incompetent compared to their former selves.
Driven by the pandemic, in the NHS and elsewhere, there has been a societal mindset change with regards to working from home. The unintended consequence of this is that a large number of menopausal women working within the NHS now have more autonomy and flexibility to manage their menopausal symptoms at home and continue to work. Interview participants were largely positive about this flexibility but did highlight that working from home allowed them to hide their symptoms from colleagues.
However, the NHS is a provider of health and care services; our analysis finds that nine of the ten women who are NHS employees of menopausal age, work in acute or mental health trusts. Three in ten women who are NHS employees of menopausal age, are nurses, health visitors and midwives. Therefore, many of those in front-line operational, clinical, medical, scientific, therapeutic or technical roles have limited options to work from home (possibly for administration tasks or meetings). Participants in such roles also reported that they welcomed the opportunity to work for home when their roles allowed them too. They also praised their colleagues who supported them to make adaptations to their usual tasks when they were impeded by symptoms (such as joint pain).
However, some participants in front-line roles described how they compromised their own personal care whilst providing patient care. Those who wore uniforms reported that the material and thickness of their uniform made their symptoms, such as hot flushes, more difficult to manage. Many participants, and this was most pressing for frontline staff, also described their strategies to deal with heavy or unpredictable menopausal bleeding. Clinical and medical staff reported that they could not always access a toilet when they needed to, either because they were seeing patients in the community, or they were pressured for time in busy clinics.
The severity of menopause related symptoms can affect how individuals participate in the NHS workforce. Our analysis suggests one in 85 NHS employees may leave their NHS roles and one in 48 may reduce their hours because of the severity of their menopausal symptoms. Some participants in the qualitative study revealed that they demoted themselves as a strategy to achieve a better work and health balance. However, given over half of female employees of menopausal age are likely to be earning less than £30000, many do not have the option to leave, reduce their hours or even demote themselves to a role with less responsibility.
What then of the menopausal women who stay in the workforce? Our triangulated analyses suggest that they either:
- Take sickness absence leave. We find that in women aged 45-54, the sickness absence rate is affected by salary, type of organisation and staff group. Our findings also suggest that menopause-related sickness is likely to be under-reported as many choose not to disclose their symptoms to their line manager or their employer.
- Continue to work whilst unwell (presenteeism) with menopausal symptoms. We find that presenteeism amongst those experiencing menopausal symptoms is linked to both personal work ethic, workload pressure (for themselves and colleagues) and perceptions of everyone else coping or sickness absence being viewed negatively by others.
Using available data we were able to model the cost for the NHS as an employer for the staff group of ‘nurses, health visitors and midwives’ and estimate this to be £116 million annually. However, this does not take into account the cost related to unproductive time of presenteeism.
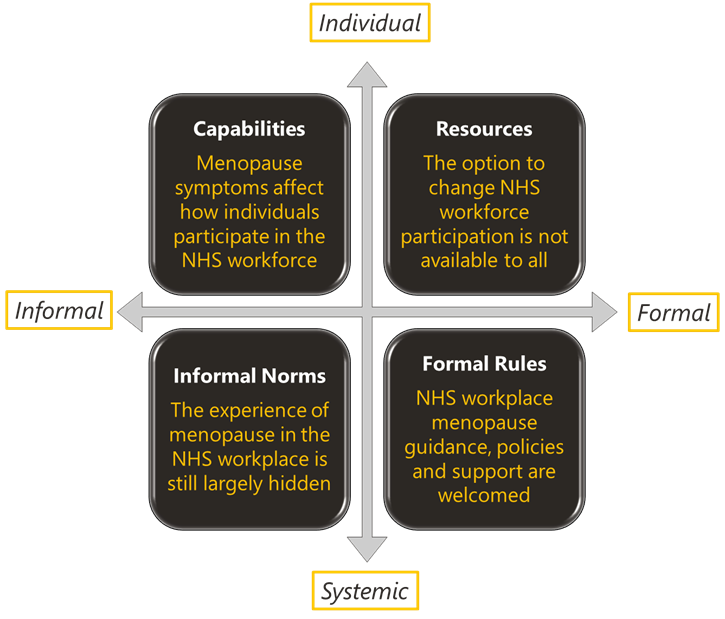
This report and the underpinning analyses describes for the first time the extent of how the menopause and its symptoms impacts on a large health and care workforce (and may be generalisable to other settings too). The findings reveal that the current status quo is an interplay of personal experiences and feasible options available to the individual which then have to be navigated within societal and institutional norms and rules (see figure above).
Recent NHS strategies (such as the Women’s Health Strategy) and guidance (such as those for line managers and colleagues) are very welcome but more focused efforts are needed across the NHS to:
- Collect, record, and analyse data related to the menopause in the workplace and then act on it
- Use clinical and medical expertise to raise awareness of the menopause in the workplace and how it can be managed at work
- Prevent the skills and expertise drain associated with the menopause, examining both the employer and personal costs
A full set of recommendations are available in the report.
CC BY-NC-ND 4.0

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.