Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive. By predicting the risk of future adverse events, we should be able to target efforts to avoid/mitigate them. Doing so would save both money and misery.
But, as Niels Bohr said wryly, “Prediction isn’t easy, especially about the future”. And the challenges of prediction increase as the thing we are trying to predict gets less specific (e.g. the risk of emergency admission in general). The challenges associated with risk stratification are nearly as great as its promises.
And risk stratification has also suffered some misguided enthusiasm. As a tool it has been over-promoted and over-sold. It is frequently sold with no sense as to how it must work: of how risk stratifying might lead to better care and so better outcomes.
Risk stratification is a means to an end. A tool like any other. And it needs to be assessed as such. So the question we asked ourselves for the short paper (below) is how might a commissioner of such tools assess the likelihood of them delivering good value?
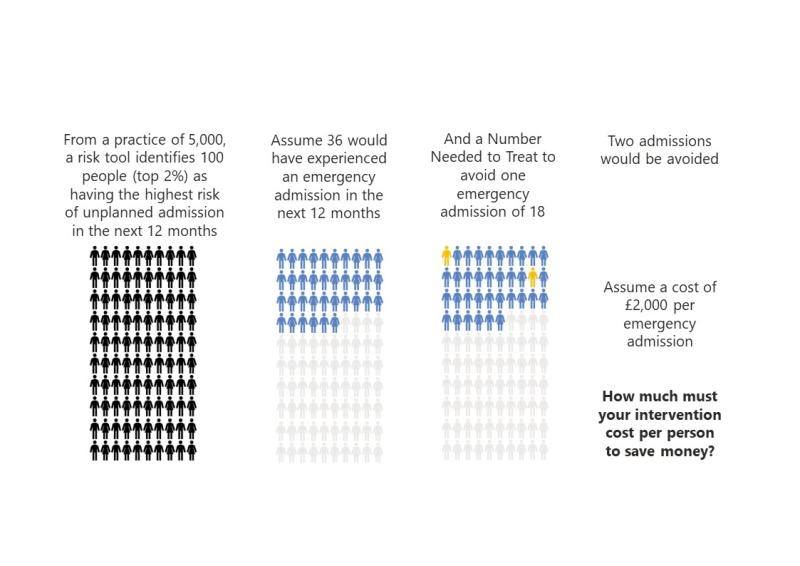
Assessing this involves a basic understanding of how risk prediction works, and the implications of that for designing any initiative. And that is the key thing: risk stratification only becomes an intervention when its results trigger action. It only becomes a useful intervention when that action delivers benefits that outweigh the costs. This is a basic equation.
In the paper we elaborate on this equation, bringing these concepts together into a simple framework. Our contention is fourfold:
- Risk stratification is a tool that can be valuable, just not in all situations.
- Anyone considering using risk stratification should consider the equation that we have put forward. They should do this before pressing ‘go’, committing time and resources.*
- All systems should have analysts that: understand how risk stratification works; can help in its technical assessment; can help weigh it against other approaches (of which there are several).**
- Any system leader involved in commissioning a risk stratification approach should ensure they understand the key concepts behind it and that they can ask the right questions to assess fitness for purpose.
We recognise that this is somewhat counter to prevailing wisdom and practice. So we’d like to hear what you think!
The paper is short and has recently been published in the BMC. It offers insights for commissioners and system leaders, aiming to help them evaluate the true value and potential of these tools in delivering better care outcomes. The NHS currently invests substantial sums (and hopes and dreams) in this tool. So considering the ideas in this paper seems a potentially valuable investment.
* Our design stage evaluation formula for risk prediction tools (as explained in the paper) combines the positive predictive value (PPV) with the number needed to treat (NNT) with the cost of the adverse event that we seek to avoid
** The Midlands Decision Support Network (MDSN) is working with analysts and leaders to develop in their local Decision Support Units (one in each ICS) the skills and the confidence in understanding to address these types of question. In a world of big data, of powerful computers and of bold sales pitches this ‘getting under the bonnet’ is key to good stewardship of resources. You can discover all about the MDSN here https://www.strategyunitwm.nhs.uk/midlands-decision-support-network
CC BY-NC-ND 4.0

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.