Expectations: The hidden driver of healthcare demand
How well do we understand changing expectations and implications for the NHS?

A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.

MDSN: Community Healthcare Services
How Does Access to Community Health Services Vary Across the Midlands?

A Picture of End-of-Life Care in England
Working with Macmillan our analysis investigates who is more likely to experience poor outcomes associated with shortcomings in end-of-life care? Are there particular areas in England where those at end-of-life face significant challenges and how might the supply of services in an area be influencing these?

What’s philosophy got to do with evidence reviews?
Ever wondered how to make better use of evidence in decision-making? Follow our latest blog series to find out more about how our Evidence and Knowledge Mobilisation team can help you to make sense of and use evidence from research and practice.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

Could a peer review methodology help drive continual learning within and across local systems?
In this blog Karen describes how peer review methodologies are being used to support learning in Long COVID services.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

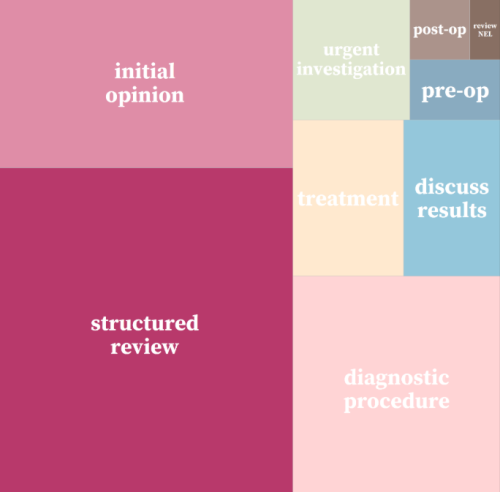
Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.
INSIGHT 2021: A new resource to support analysis of outpatient services
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.
INSIGHT 2021: Insight to Action. What Works?
It has been estimated that it can take up to 17 years to translate evidence into practice – how can we change that?

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.

Learning the lessons of Long Covid in real time
Round table event, 12 July
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.

Making sense of evidence
It's time to celebrate World Evidence-Based Healthcare (EBHC) Day. In a world dominated by COVID-19 and the associated infodemic, this day arguably has more resonance. Closer to home, EBHC Day also coincides with our Insight 2020 festival and the launch of the Midlands Decision Support network. What better opportunity to ask, 'what does evidence-informed decision making actually mean'?
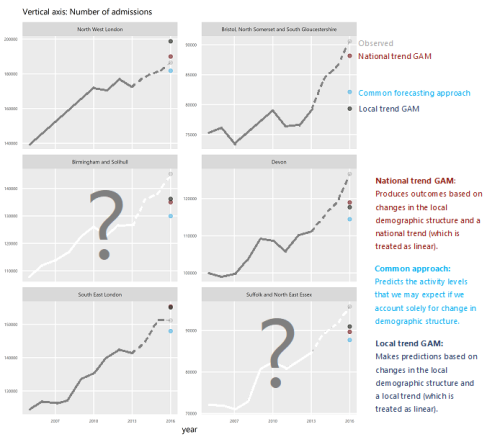
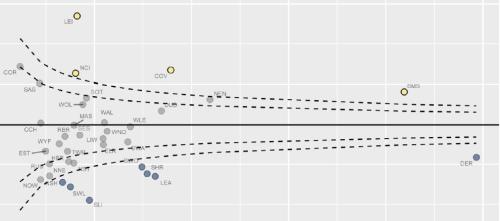
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.