
Expectations: The hidden driver of healthcare demand
How well do we understand changing expectations and implications for the NHS?
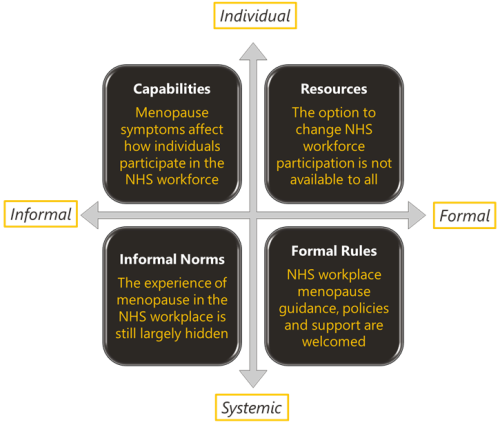
Menopause and the NHS workforce
The impact of the menopause on the NHS workforce. The Strategy Unit and Health Economics Unit report on their mixed methods findings.

Learning about what works in urgent community response
The initial report from the national urgent community response (UCR) evaluation, along with an economic modelling tool to help service providers and systems understand the impact of UCR, is now available.

What’s philosophy got to do with evidence reviews?
Ever wondered how to make better use of evidence in decision-making? Follow our latest blog series to find out more about how our Evidence and Knowledge Mobilisation team can help you to make sense of and use evidence from research and practice.

Could a peer review methodology help drive continual learning within and across local systems?
In this blog Karen describes how peer review methodologies are being used to support learning in Long COVID services.

The NHS as an anchor institution: addressing fuel poverty
The number of households in fuel poverty in Staffordshire and Stoke-on-Trent (SSoT) is higher than the national average. As anchor institutions, NHS organisations can use their assets to influence the health and wellbeing of their local communities. The Strategy Unit was asked by the Midlands NHS Greening Board to evaluate a cross-sector initiative in SSoT to help alleviate fuel poverty using savings generated through solar panels on NHS buildings. The project is called Keep Warm, Keep Well.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).
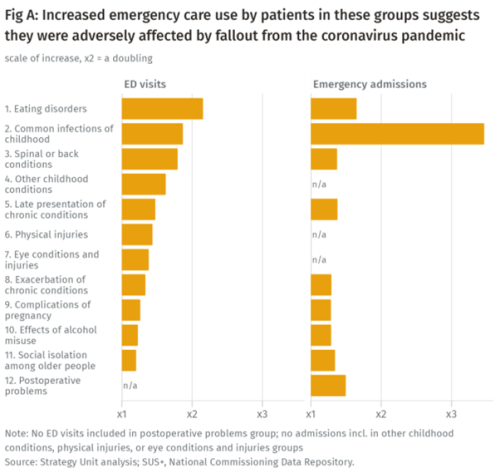
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.
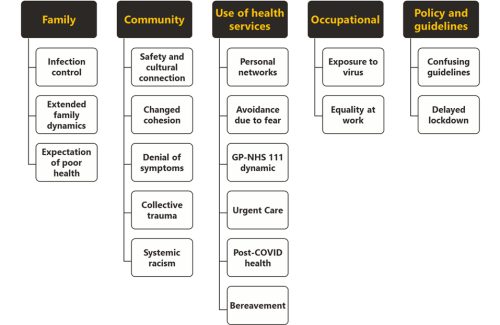
We don’t just need to hear ‘you are more affected’ - what’s the action?
The experience of minority ethnic people symptomatic for COVID-19 in the first UK wave of the pandemic.
INSIGHT 2021: Insight to Action. What Works?
It has been estimated that it can take up to 17 years to translate evidence into practice – how can we change that?

Measuring the effect of the coronavirus pandemic on population health
Measuring the effect of the coronavirus pandemic on population health

Learning the lessons of Long Covid in real time
Round table event, 12 July

Increasing vaccine uptake
The purpose of this work was to identify the key features of local initiatives which encourage vaccine uptake in different population groups, and share these for others to learn from.

Making sense of evidence
It's time to celebrate World Evidence-Based Healthcare (EBHC) Day. In a world dominated by COVID-19 and the associated infodemic, this day arguably has more resonance. Closer to home, EBHC Day also coincides with our Insight 2020 festival and the launch of the Midlands Decision Support network. What better opportunity to ask, 'what does evidence-informed decision making actually mean'?

Have cuts to public spending on social care for older people led to more emergency hospital admissions?
Cuts to council social care budgets are often cited as a cause of pressure on NHS urgent and emergency care services. Much of the evidence supporting this link, however, is anecdotal. We set out to try and quantify the effect of cuts to social care on older people’s use of emergency healthcare services, and our research has just been published in BMJ Open.
New care models - what's the evidence
High level findings from a series of evidence reviews on new care models.
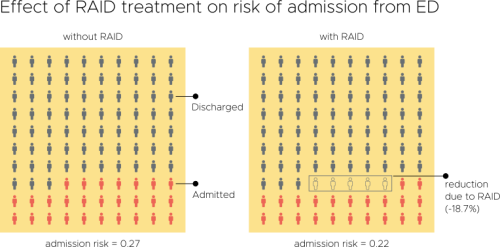
Evaluation of an Integrated Mental Health Liaison Service (Rapid Assessment Interface and Discharge Service) in Northern Ireland
A high proportion of patients treated for physical health conditions also have co-morbid mental health problems; and there is growing acceptance of
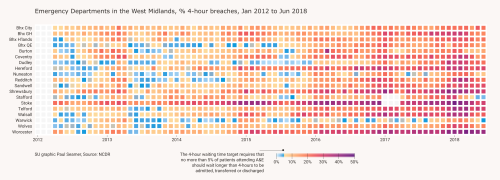
New Perspectives on the Perennial Problem of Urgent Care
Waiting times in A&E are never far from the headlines. It threatens to become the defining healthcare performance issue of our time
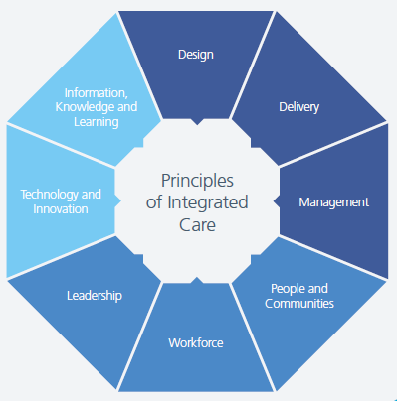
Integrating health and care services - what works? It’s complicated…
Coinciding nicely with the NHS 70th Birthday celebrations and the parallel discussions of ‘where next and how to do it better’ for the NHS, last we

What works for primary care led integration?
We recently shared highlights from our realist synthesis on primary care-led integrated models, at the Health Policy and Planning Network workshop. Take a look at our presentation for a flavour of our findings ahead of publication later in the summer.