
Heart Failure Targeted Funding Programme 2023/24 Evaluation
The Heart Failure Targeted Funding Programme was an NHS England initiative to improve access to heart failure specialists in the commu

A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.

Hydration, UTIs and older people: learning from NHS pilots about how to improve care
Our evaluation of hydration-focused interventions for older people found promising signs of impact and highlighted the practical and systemic challenges of delivering and sustaining change.

Virtual wards: Patient and unpaid carer experiences of ‘hospital at home’ care
Our evaluation of patient and carer experiences of virtual wards found widespread benefits and highlights areas for improvements parti

MDSN: Community Healthcare Services
How Does Access to Community Health Services Vary Across the Midlands?

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.
MDSN: GP practice productivity, efficiency, and continuity of care
GP Practice productivity, efficiency, and continuity of care
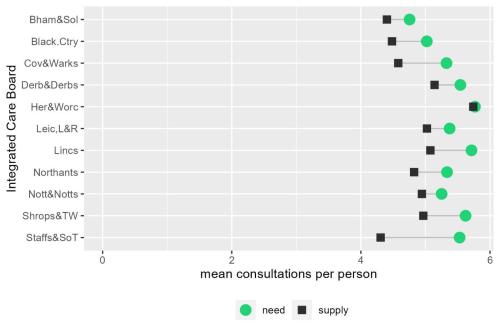
MDSN: The gap between need and supply of GP practice consultations
The gap between need and supply of GP practice consultations
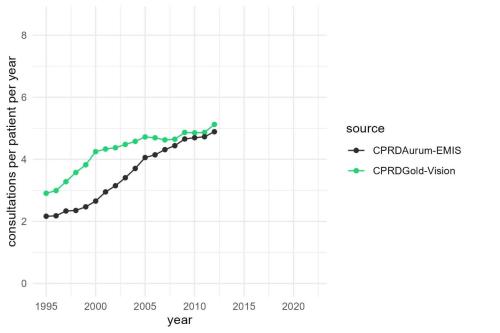
MDSN: Long-term trends in GP practice Consultation Rates
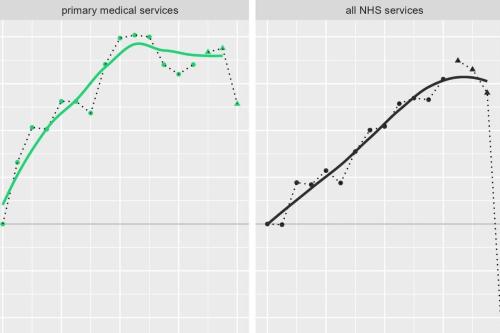
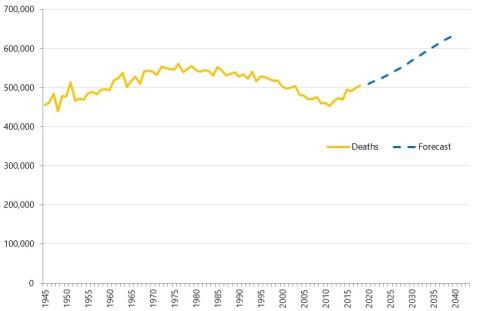
GP practice consultations are, by some distance, the most common interaction between the NHS and the population it serves.

Review of Ophthalmic Managed Clinical Networks (MCNs) in Staffordshire and Shropshire
The aim of the MCNs is to bring together primary care optometrists with local ophthalmologists within a geographical area. This is a review Strategy Unit were commissioned by NHS England to work with a medical retina MCN in Shropshire, Telford and Wrekin and a glaucoma MCN in Staffordshire and Stoke on Trent, to review their work so far and look at the opportunities the networks present.

Learning about what works in urgent community response
The initial report from the national urgent community response (UCR) evaluation, along with an economic modelling tool to help service providers and systems understand the impact of UCR, is now available.
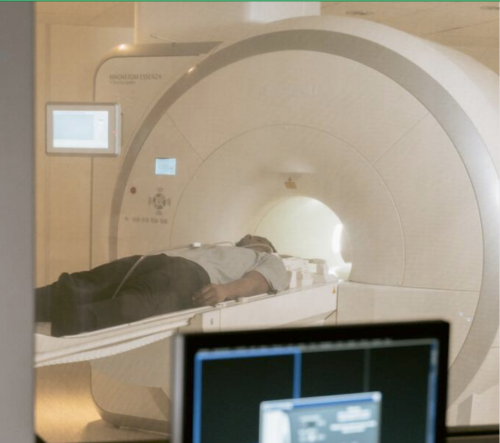
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
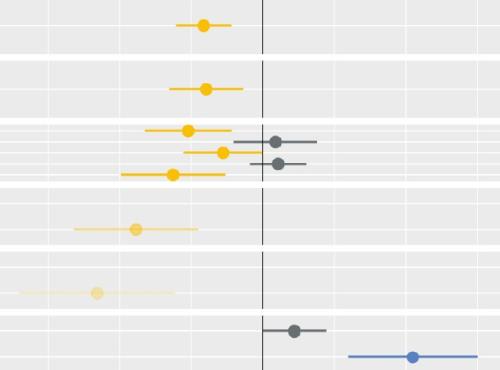
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

Strategies to reduce inequalities in access to planned hospital procedures
UPDATE 10th August: Now including briefing note for Integrated Care Boards on legal duties in respect of reducing inequalities. This report guides ICBs through the process.

What do we know about the benefits of digital social care records?
The pace of change in the development and use of digital technology is astonishing. The use of such technology has been an essential element in the health and care services response to the COVID-19 pandemic. In many cases, the previously unthinkable became commonplace.

Increasing vaccine uptake
The purpose of this work was to identify the key features of local initiatives which encourage vaccine uptake in different population groups, and share these for others to learn from.
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.

Evidence review: Early diagnosis of cancer
Detecting cancers early is essential to saving lives and reducing the need for invasive treatments.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
