GP Practice productivity, efficiency, and continuity of care
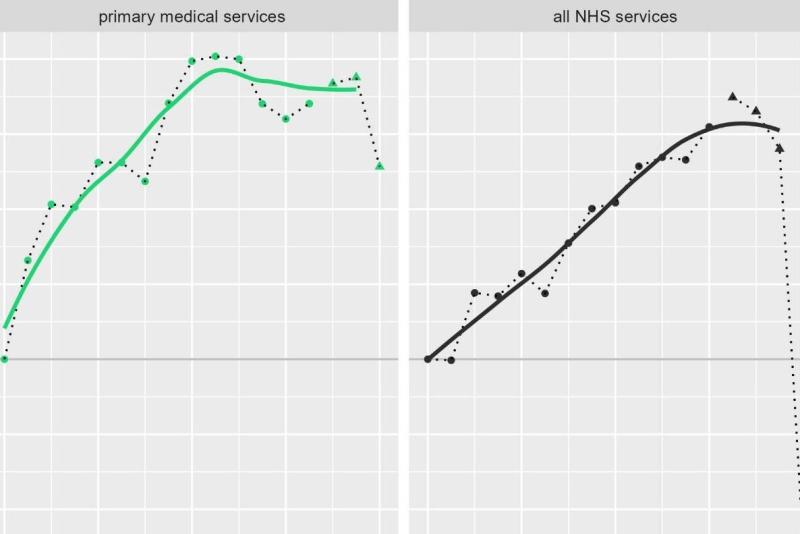
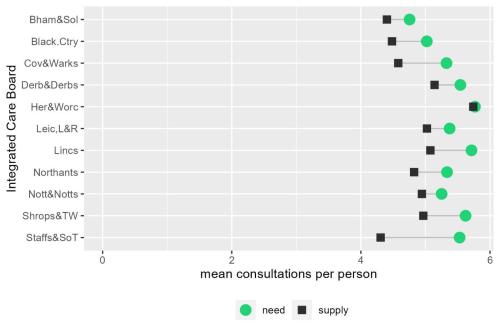
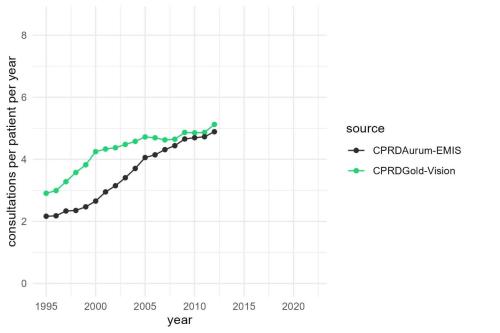
In the previous two reports in this series, we showed that crude GP practice consultation rates, the average number of consultations per person per year, has been falling since 2012, whilst the need for consultations has been increasing. A substantial gap between need and supply has opened up, with significant consequences for patients and the wider health system. Almost half of patients now report difficulty getting through to their GP practice by telephone. Attendances at over-stretched emergency departments for conditions treatable in GP practices have increased. And there has been a rise in the number of emergency admissions to hospitals for ambulatory care sensitive conditions.
The scale of the gap between need and supply is such that substantial GP recruitment must be the mainstay of any solution. But large-scale, national efforts to increase the numbers of clinical staff take time, and despite considerable efforts, the number of fully qualified, permanent GPs, the core of the primary care workforce, has fallen since 2015.
Resolving this recruitment problem remains a key feature of national strategies for primary medical services. But given the pressing consequences of an under-supply of GP practice consultations and the intractability of the GP recruitment challenge, efforts to close the gap between need and supply have increasingly focused on productivity solutions.
In this report, we explore the issue of GP practice productivity and efficiency; how it might be measured, how it has changed over time, the degree of geographic variation, and the relationship between productivity, efficiency, and continuity of care for patients. We draw heavily on three pieces of research carried out recently by the University of York, by the Strategy Unit in conjunction with the University of Birmingham and by the University of Cambridge and the INSEAD business school.
Key Findings
Analysis by the University of York suggests that cost-weighted productivity of primary medical services increased rapidly, by 2.3% per annum between 2004 and 2012. Since 2012 productivity growth has stalled.
A cross-sectional analysis of GP practice productivity in 2019 and 2020, carried out by the Strategy Unit, suggests that there is little headroom for productivity growth within the service model that was prevalent at the time.
The benefits of care continuity to patients, staff and health systems have been widely reported. But recent research by the University of Cambridge finds a positive relationship between continuity of care and the efficiency of a GP practice consultation. The time to a patient’s next appointment is increased if they are seen by their usual GP.
As efforts to increase the number of GPs have faltered, attention has turned to reducing the gap between need and supply of GP practice consultations by improving input-output productivity. These efforts take many forms including division of labour and the delegation of duties to nurses and other healthcare professionals, remote consultations, extended hours, the diversion of low acuity cases to pharmacies, and the merging and federating of GP practices.
These efforts to improve input-output productivity may be undermined by the absence of financial incentives to increase supply. They may also lead to unintended reductions in continuity of care which increases need and reduces supply.
An alternative approach to closing the gap between need and supply of GP practice consultations would make continuity of care the primary objective. A strategy based on this priority would be a radical departure from current policy.
Please have a listen to our podcast below:
CC BY-NC-ND 4.0

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.