Strengthening ethnicity data across the NHS: developing the national improvement plan
Our analysis and stakeholder engagement supported NHS England to develop the national Ethnicity Recording Improvement Plan.

Expectations: The hidden driver of healthcare demand
How well do we understand changing expectations and implications for the NHS?

Hydration, UTIs and older people: learning from NHS pilots about how to improve care
Our evaluation of hydration-focused interventions for older people found promising signs of impact and highlighted the practical and systemic challenges of delivering and sustaining change.
Why can’t I prove my programme is effective?
Evaluation blog series continues with Impact Evaluation Lead Mike Woodall looking at how programme designers can maximise the chances of success.

MDSN: Community Healthcare Services
How Does Access to Community Health Services Vary Across the Midlands?

What’s philosophy got to do with evidence reviews?
Ever wondered how to make better use of evidence in decision-making? Follow our latest blog series to find out more about how our Evidence and Knowledge Mobilisation team can help you to make sense of and use evidence from research and practice.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
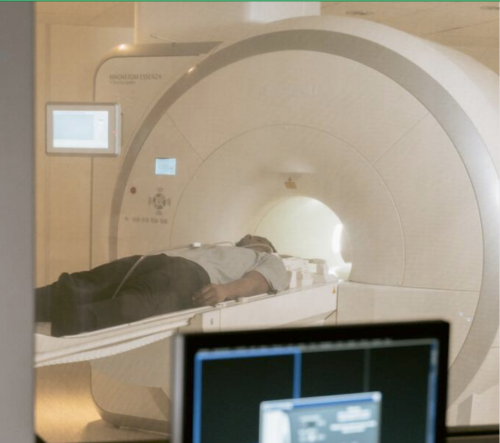
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

Could a peer review methodology help drive continual learning within and across local systems?
In this blog Karen describes how peer review methodologies are being used to support learning in Long COVID services.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).

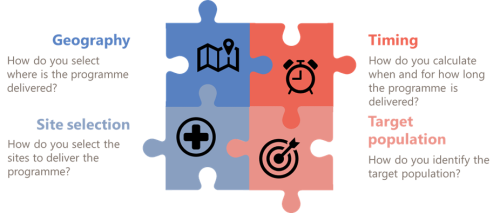
Urgent Community Response – What Works?
The Strategy Unit, with our partners Ipsos, has been commissioned by NHS England and NHS Improvement (NHSEI) to provide a long-term national evaluation of the Urgent Community Response programme rolled-out across England. The programme aims to shift resources to home and community-based services as part of the NHS commitment to providing the right care, to the right people, at the right time. And there are a range of outputs from the early work that provide learning for local systems as they develop their services.

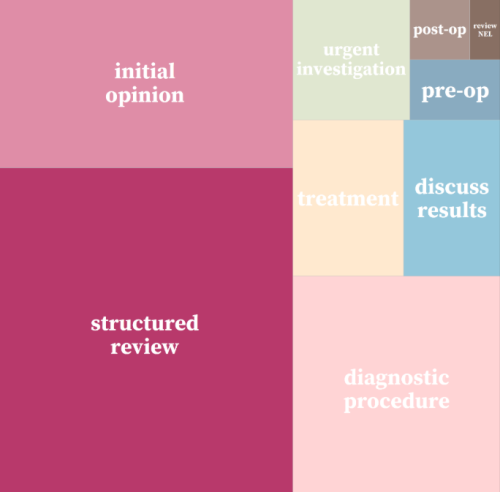
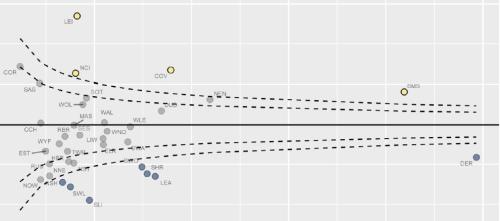
Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.
INSIGHT 2021: A new resource to support analysis of outpatient services
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.
INSIGHT 2021: Insight to Action. What Works?
It has been estimated that it can take up to 17 years to translate evidence into practice – how can we change that?

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.

Learning the lessons of Long Covid in real time
Round table event, 12 July

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.