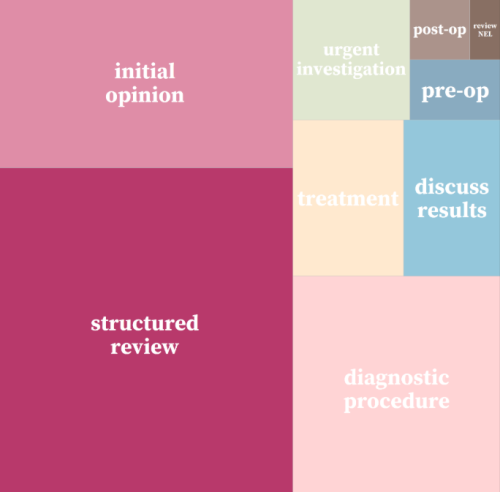
Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.

INSIGHT 2021: The most valuable value - a health and care resourcing dilemma
We heard discussions from experts from the NHS, NICE and academia (Andi Orlowski, Gwyn Bevan, Deborah O’
INSIGHT 2021: A new resource to support analysis of outpatient services
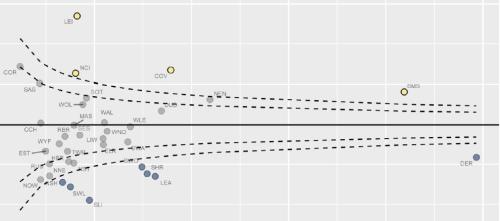
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.
INSIGHT 2021: What can we learn from the pandemic to reduce health inequalities
The COVID pandemic has highlighted the stark inequalities in health that exist in the UK and globally.
Insight 2021: Welcome to INSIGHT 2021
Peter Spilsbury (Director, Strategy Unit) welcomes you to INSIGHT 2021 and i

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.
Evaluating Artificial Intelligence: a significant new win
The Strategy Unit, the Health Economics Unit and Leicester Clinical Trials Unit have been announced as evaluation partners to support success in the Artificial Intelligence (AI) in Health and Care Awards.

A learning NHS and ‘black box’ analysis aren’t compatible
Data analysis presents a limitless opportunity to improve decision making within the NHS.
The bigger picture
Today, the Health Foundation launched the REAL Centre (Research and Economic Analysis for the Long term), an incredibly important initiative to imp
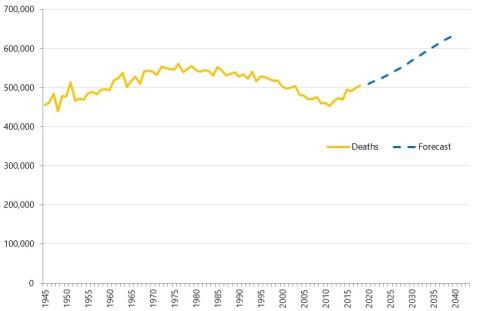
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
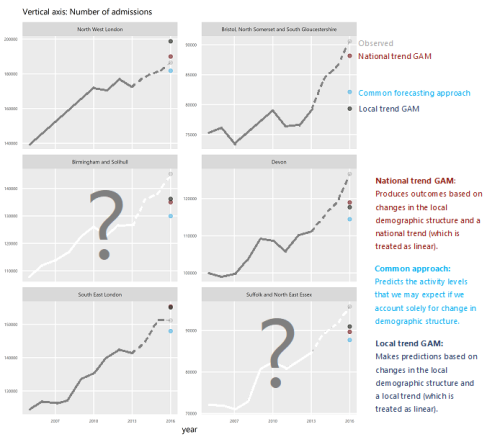
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.

Why community alternatives to hospital admission don’t (typically) reduce total admission levels
Repeatedly, published evaluations show that community/primary care services interventions with a stated intention to reduce total (or forecast total) emergency admissions to hospital don’t achieve the expected result**
Part of the solution or part of the problem? Management Consultants and the NHS
I was quoted in a recent Guardian newspaper article which described a London Clinical Commissioning Group’s wasteful use of external
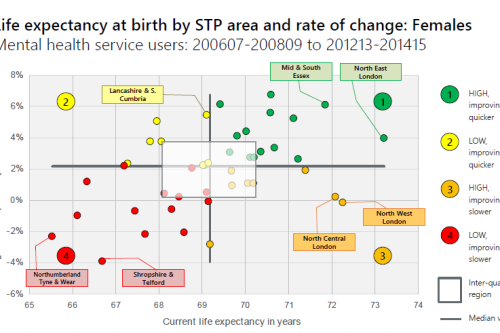
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20
Mental Health and integration: Cinderella or the Ugly Sisters?
Introduction
Do you like to integrate horizontally or vertically? NHS positions examined
Our latest research paper explores the impact of the different options for integration implemented as a result of the Transforming Community Services policy in 2010. This accompanying commentary reflects on potential implications for the current policy drive towards Integrated Care Systems.
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally integrate with a mental health trust, or set up a stand-alone community trust or Community Interest Company? Seven years on, this report explores the impact this choice had on the level and growth in emergency hospital use in older people and considers the wider implications for the NHS as it develops new models of care and integrated care systems