
Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.
Contracting for health outcomes: from concept through theory to implementation
In this new report, jointly authored with colleagues from the University of York and The Royal Orthopaedic Hospital NHS Foundation Trust, we set out in detail how an outcomes-based contract for elective knee replacements might be constructed, and the potential implications for commissioners, providers, and policy-makers.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
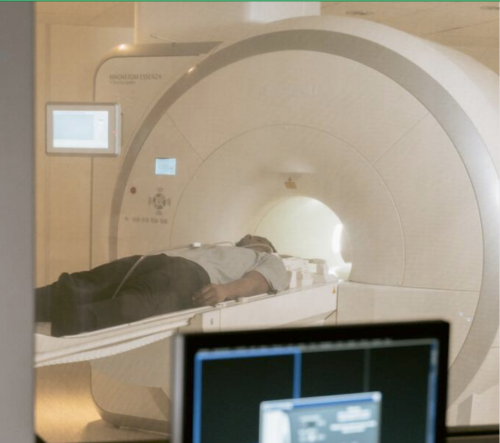
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

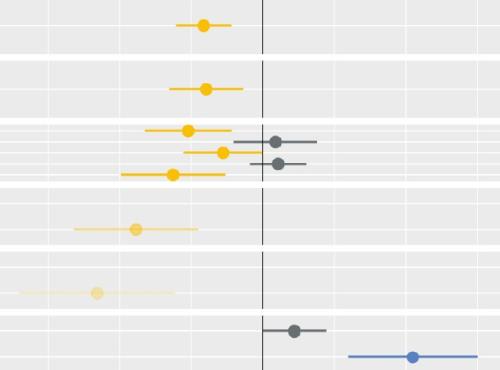
Helping ICSs to reduce inequalities in access to planned care
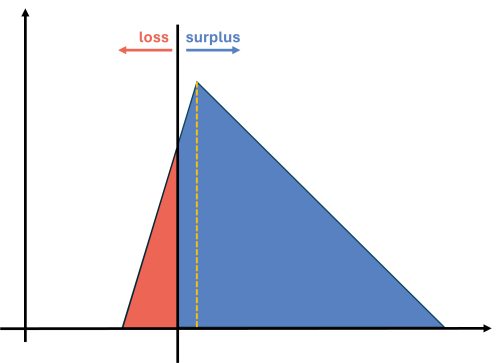
Are there inequalities in access to planned care? If so, what are they? Which groups ‘gain’ and which groups suffer? And what could be done to address any inequalities? In pursuing their objective of reducing inequalities, what could Integrated Care Systems (ICSs) do? What strategies and approaches are likely to be successful?

Inequalities in access to healthcare - what’s our next move?
Our research, published in the Lancet Regional Health Europe, highlights substantial inequities in access to elective hip replacement surgery. We found no evidence that these inequities reduced between 2006 and 2016.

Strategies to reduce inequalities in access to planned hospital procedures
UPDATE 10th August: Now including briefing note for Integrated Care Boards on legal duties in respect of reducing inequalities. This report guides ICBs through the process.

Treating people on waiting lists: who decides what is fair?
Waiting lists for elective care are in the news. The national plan has been issued, with the expectation that lists will continue to rise for some years - and that long waiting will not disappear anytime soon. Addressing this ‘backlog’ will remain a fundamental challenge for some time to come.

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
Modelling the impact of covid on waiting lists for planned care
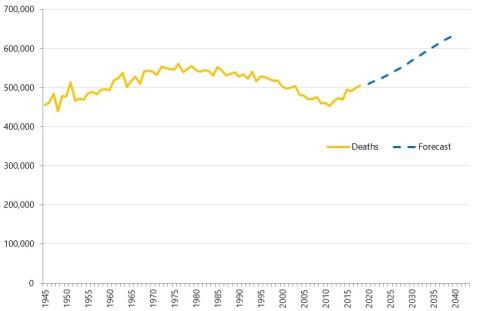
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.
Scoping the Future (CRUK)
Within the context of rising demand for diagnostic services and concerns about capacity, Cancer Research UK commissioned this project to explore the issues for endoscopy services, to inform national strategic recommendations.