Are there inequalities in access to planned care? If so, what are they? Which groups ‘gain’ and which groups suffer? And what could be done to address any inequalities? In pursuing their objective of reducing inequalities, what could Integrated Care Systems (ICSs) do? What strategies and approaches are likely to be successful?
Over the last year, the Strategy Unit has been looking at questions such as these. Our initial work was commissioned by the 11 ICSs that make up the Midlands Decision Support Network but the results apply to the whole NHS.
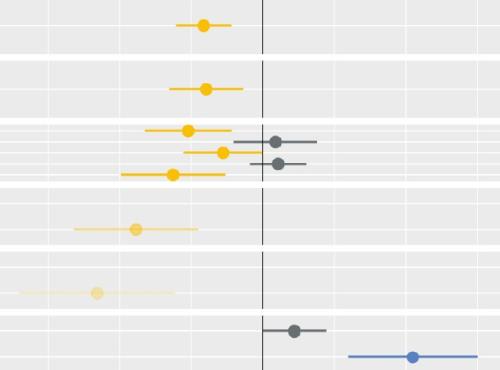
Our reports show that inequalities are considerable and that actions taken during lockdown widened these further. We showed that inequality arises later in the pathways of care, more than has been recognised to date. We also suggested that systems will have to redistribute resources between population groups. We highlighted serious problems that require similarly serious, and potentially contentious, actions.
Our first report examined the problem. It showed the causes and consequences of inequalities in access to planned care.
The second report asked what could be done. Having defined the problem, what could ICSs do to address it?
Healthcare resources are finite. Deciding to distribute these resources is a fundamental responsibility of system leaders.
To be blunt, if systems aren’t doing that, then it’s unclear what they are there for. Keeping the status quo is as much a decision as changing it – there is no neutral position.
And all choices rest on value judgements (framed by legal obligations). There is no technocratic ‘right answer’. Instead, there are multiple possibilities – each of which can be supported and disputed from different value-based standpoints.
ICSs need sophisticated and high-quality analysis to support their considerations. But this is not enough. They also need to consider the legitimacy they have for responding to inequalities through redistribution, and the processes they adopt when making such decisions.
This isn’t easy. And it perhaps explains why despite repeated – and genuinely meant - statements of intent, in reality the accumulation of policy and performance imperatives over the last ten years has led to a greater proportion of NHS elective resource being used to serve the least disadvantaged groups in the population.
To try to support ICSs in thinking about how they can break the mould, we have therefore commissioned some further work that we bring together here alongside our original reports.
The first piece of work looks at legal responsibilities. In our experience, there has been some confusion amongst leaders about what the law allows/requires when it comes to addressing inequalities. So we commissioned colleagues at Hill Dickinson LLP to summarise the current legal duties of Integrated Care Boards (ICBs) – and to review all of the potential strategies we have set out through that legal lens.
The resulting report is powerful. It shows that meeting legal obligations requires a strategic approach along the lines suggested in our report, and that the current legal position requires authorities to give the same attention to socioeconomic inequalities as to those for other protected characteristics. The report is HERE.
The second piece of work concerns the views of citizens. When considering legitimacy for value-based decisions, it is essential that organisations/systems explore the views of the public they serve. To do this thoroughly requires investment in well-designed and carefully conducted deliberative processes. We owe it to those we consult to give them the time and space to gather evidence and to go on a journey of exploration in reaching views on complex topics.
University Hospitals Coventry & Warwickshire (UHCW) NHS Trust are taking bold action in trying to address elective inequalities. They have developed a system (that is attracting widespread interest and adoption) that allows them to take into account a broader range of factors when deciding ‘how to prioritise long waiting lists based on needs’. They realise however that they need to do this with care and with due attention to the views of their public.
To help them in this and to exemplify the approach, Midlands and Lancashire Commissioning Support Unit (who host the Strategy Unit) supported a project whereby our partners Ipsos worked with the trust in conducting a deliberative process with a ‘mini population’ designed to be reflective of the local population.
That ‘mini population’ worked together over an accumulation of 12 hours to address a range of questions. Their views weren’t always unanimous and developed as the conversation progressed. The views developed by the group were nuanced, challenging some of the thinking that it is easy for organisations to slip in to.
Importantly, for example, the group drew a distinction between using population-level factors such as ethnicity and deprivation and individual risk factors, such as disability and lifestyle factors to drive efforts to address inequity. The group broadly supported population-level targeted action to improve disease identification and service take up and were less supportive of using population-level factors to make decisions about an individual’s place on waiting lists.
Professor Kiran Patel, Medical Director at UHCW, offers his perspective on the work in his blog HERE and we are pleased to publish the Ipsos report HERE. Our hope is that this prompts others to consider how best to have such conversations with their local populations.
The Strategy Unit is committed to working to reduce inequalities in health and healthcare. This is a huge challenge for system leaders requiring the weighing up of multiple factors and lines of thinking alongside well designed decision-making processes. We invite anyone else working on inequalities to get in contact and to share work and ideas for further work that can actually make a difference in this endeavour.