
Planning for rising renal demand: simulating capacity across the care system
Demand for kidney replacement therapy is rising, and current capacity will not be sufficient over the next decade. This work uses simulation modelling to help systems understand future pressures and test potential responses.

Beating the backlog: Meeting the waiting list challenge
The NHS waiting list in England must halve to reach waiting time targets.

The Strategy Unit contribution to neighbourhood health
Our role in supporting the national effort to turn the vision of neighbourhood health into action by providing evidence, analysis and insight.
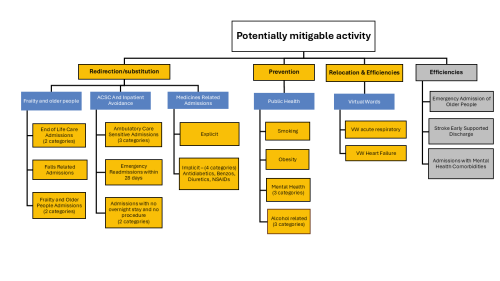
Shifting care ‘from hospital to community’: where to start?
What are the opportunities to shift activity from hospital to community? Our analysis provides an evidence-based place to start.

A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.
Strategy Unit demand model wins prestigious Florence Nightingale Award
Our open-source demand model, developed in collaboration with the New Hospital Programme, has been named the 2025 winner of the Florence Nightingale Award for Excellence in Health and Care Analytics.
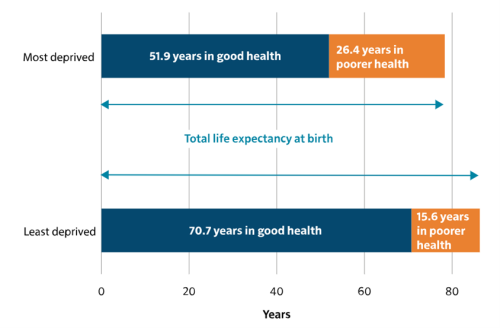
Things can only get better (?)
Introducing a new online tool to help local health and care service planners think differently about healthy ageing.
Transforming Hospital Planning with an Open-Source Demand and Capacity Model
We are proud to announce the open-sourcing of a demand and capacity model, developed with the New Hospitals Programme, to transform NHS hospital planning with transparency, collaboration, and efficiency.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.
Midlands Analyst Network and Huddles
The Midlands Analyst Network was created to provide a space for analysts to share information, ideas and resources, as well as seek advice and guidance from one another.

Part-time GPs and the decline in continuity of care: a cause or a symptom?
In our recent paper we explore why levels of care continuity have been declining and what might be done to turn things around.

Two sides of the same coin
Hospital demand arising from GPs not seeing patients, is eating into the resources that they would use to manage down the elective backlog. In turn, this is creating more demand for GPs.

Are GP consultation rates rising or falling? Who or what should we believe?
If the "data suggests" GP appointments are substantially higher than pre-pandemic, then what is behind patients reporting recieving fewer appointments?

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.

A collaborative partnership with the Health Foundation
The Strategy Unit is collaborating with the Health Foundation to help address key health and social care issues by combining our expertise in data analysis.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
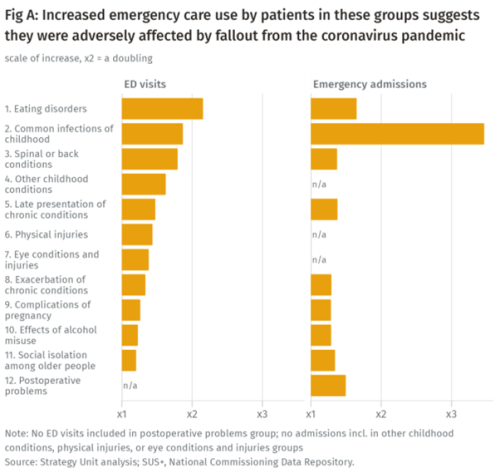
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.

Bringing patient flow modelling into general practice
With general practice appointments hitting the highest numbers on record (34.8 million in England alone in November 2021), careful organisation and planning for patient appointments is increasingly important.