
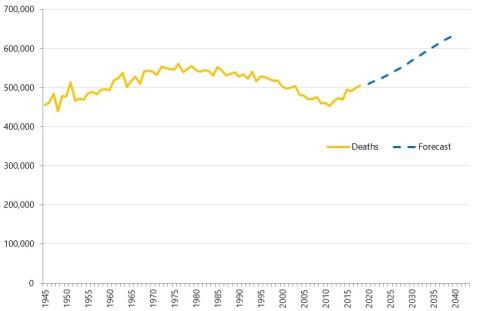
What explains the recent growth in hospital activity?
In this long read, Fraser Battye describes our analysis of what has driven the growth in hospital activity.
Strategy Unit demand model wins prestigious Florence Nightingale Award
Our open-source demand model, developed in collaboration with the New Hospital Programme, has been named the 2025 winner of the Florence Nightingale Award for Excellence in Health and Care Analytics.
Transforming Hospital Planning with an Open-Source Demand and Capacity Model
We are proud to announce the open-sourcing of a demand and capacity model, developed with the New Hospitals Programme, to transform NHS hospital planning with transparency, collaboration, and efficiency.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘Internal Consultancy’: INSIGHTS from evidence and experience
In this blog, our Head of Policy, Fraser Battye, shares his reflections on a recent ‘SU INSIGHTS’ event on the ‘Internal Consultancy’

From ‘right drift’ to ‘left shift’?
Our Head of Policy, Fraser Battye, looks at the challenges facing the intention to shift care ‘from hospital to community’. He suggests that we have missed a critical part of the explanation for why this ‘left shift’ hasn’t taken place following previous initiatives.

Charisma
In this long read, which first appeared in the HSJ, Fraser Battye - our Head of Policy – looks at the role of charisma and innovation in the way that NHS resources are allocated.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.

Ara Darzi, Wes Streeting and English health policy. Part 2: cutting the knot
Following on from part one, Fraser continues exploring the Gordian Knot of English health policy.

Ara Darzi, Wes Streeting and English health policy. Part 1: the Gordian Knot
Health policy is not at a crossroads, it is in a bind. Strands so entangled, so complex they resemble a Gordian knot. Can this knot be untied?

Want to ease pressure in urgent care? Simply cut community services!?!
What should decision makers do with analysis that challenges deeply held assumptions? In this blog, Fraser Battye reflects on a surprising recent finding about community services.

Ghosted by an old friend
“…personal contact was a vital element in general practice from the beginning. By 1959 50% of people in England regarded their GP as a personal friend.”

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
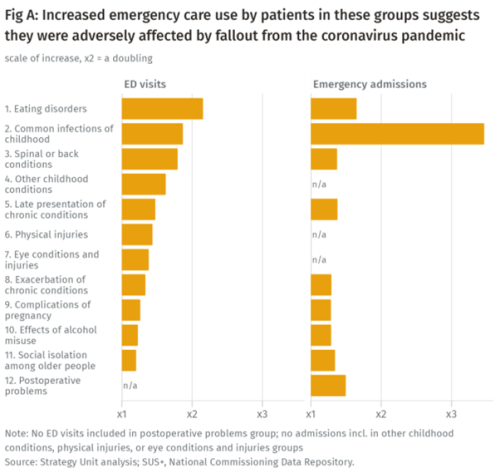
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.

Urgent Community Response – What Works?
The Strategy Unit, with our partners Ipsos, has been commissioned by NHS England and NHS Improvement (NHSEI) to provide a long-term national evaluation of the Urgent Community Response programme rolled-out across England. The programme aims to shift resources to home and community-based services as part of the NHS commitment to providing the right care, to the right people, at the right time. And there are a range of outputs from the early work that provide learning for local systems as they develop their services.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.
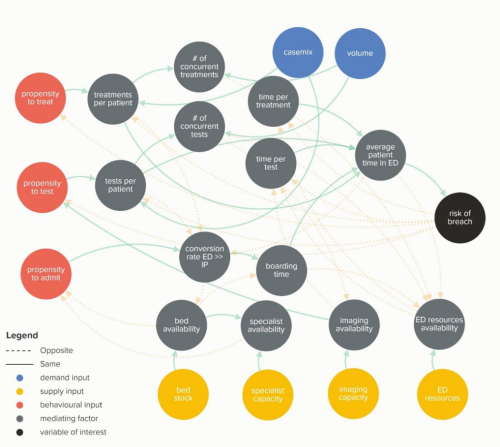
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.