A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.

Mending smarter, not harder: Changing fracture care for children
The report demonstrates there is significant variation between trusts in England in how paediatric fractures are managed. Widespread adoption of less interventional approaches to paediatric fracture management could result in significant savings in hospital activity, particularly reduced follow-up appointments for uncomplicated fractures.

“Champion, challenge, collaborate.”
Being commissioned by the Mayor of London to produce independent reviews of proposals for major service change, affecting Londoners, perfectly aligns with our commitment to help the health and care system make better decisions and ultimately achieve benefits for population health and wellbeing.

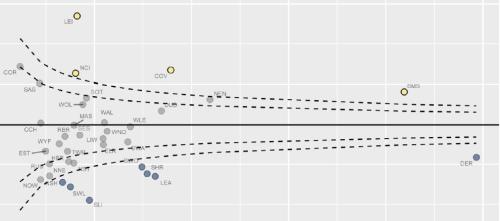
MDSN: Community Healthcare Services
How Does Access to Community Health Services Vary Across the Midlands?

A Picture of End-of-Life Care in England
Working with Macmillan our analysis investigates who is more likely to experience poor outcomes associated with shortcomings in end-of-life care? Are there particular areas in England where those at end-of-life face significant challenges and how might the supply of services in an area be influencing these?

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.

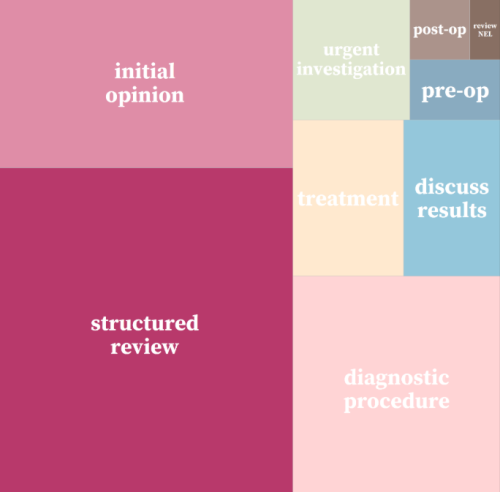
Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.
INSIGHT 2021: A new resource to support analysis of outpatient services
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.

Inequities in children and young people’s mental health services
Good mental health during early years and childhood has a great bearing on health throughout life.

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
Strategy Unit analysis of air quality highlights inequalities
Poor air quality is the largest environmental risk to public health in the UK and central London has the highest levels of particulate matter and nitrogen dioxide. The Guy’s and St. Thomas’ charity, now operating its programmes under the Impact on Urban Health banner, have committed to 10 years of funding to improve air quality-related health in the residents of South London boroughs of Lambeth and Southwark. The charity commissioned the Strategy Unit to explore the health of several key groups and the factors that most influence health alongside air quality within the area.
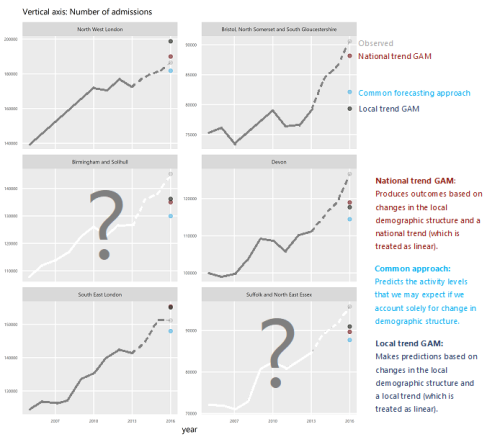
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.
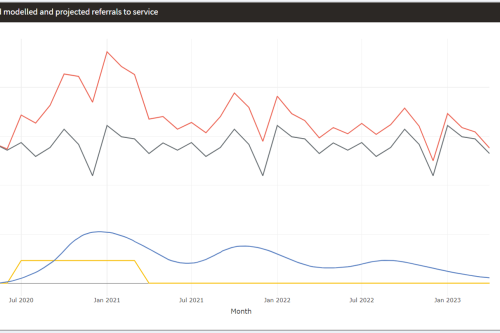
Mental Health Surge Model
Early in the Covid pandemic, it became clear that people’s mental health would suffer. Whether through bereavement, unemployment, social isolation, not being able to access support services – or a host of other routes – an alarming picture began to emerge and attract attention.
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.
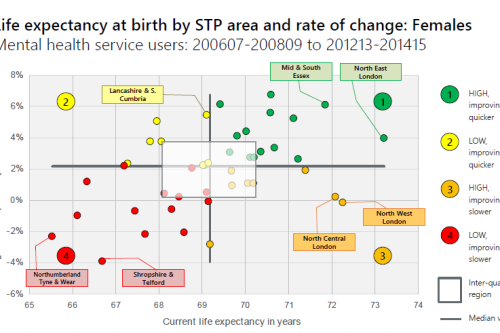
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20