Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.

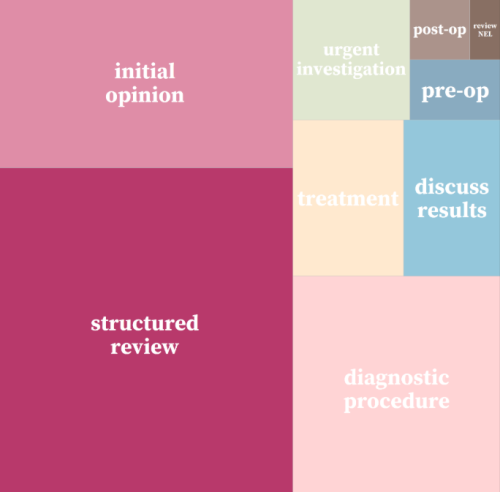
Strategy Unit devises a new method for classifying outpatient appointments
The number of outpatient attendances in England is now approaching 100 million each year.
INSIGHT 2021: A new resource to support analysis of outpatient services
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department

Emergency Department attendances reach new high – August may bring new challenges
Earlier this year, the Str

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
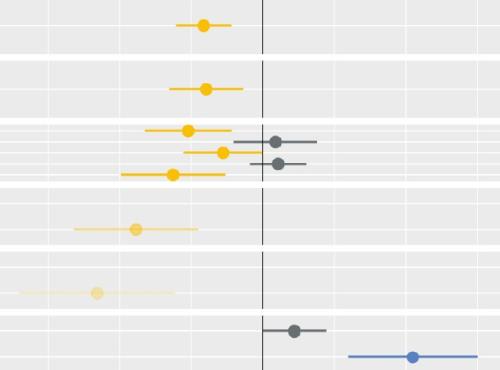
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.

A framework for understanding policy change
A new policy, strategic direction or major programme is announced.

Localism and the NHS: a case in four stories
In this blog, Fraser Battye makes the case for localism in the NHS. He tells four short stories. He suggests that these stories highlight an opportunity as the NHS enters a period of reform.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of

Learning from lockdown: support for people experiencing homelessness
There are few clearer measures of societal health than homelessness.

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
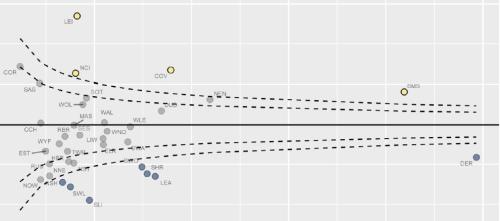
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.

Is ‘Integrating Care’ bold enough?
In this blog, Fraser Battye leaves the Strategy Unit’s usual careful and empirical view of the world. He reflects on NHS England and Improvement’s ‘Integrating Care’ paper from the perspective of wider ideological and societal trends. In doing so, he suggests that there is scope for bolder reform – and that localism is the way to go.
What might ‘Integrating Care’ mean for analysts?
In this blog, Fraser Battye looks at NHS England/Improvement’s ‘Integrating Care’ paper. While not looking forward to another NHS re-organisation, he sees a lot that analysts will like. Fraser also notes the potential advantage that the Decision Support Unit model gives systems in the Midlands. What can analysts do to seize these opportunities?
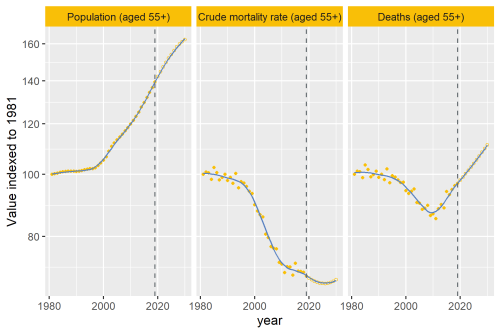
Why are deaths set to rise?
In our recent analysis of healthcare use in the last 2 years of life, we point out an important change that’s taking place to life and death in the UK.
The bigger picture
Today, the Health Foundation launched the REAL Centre (Research and Economic Analysis for the Long term), an incredibly important initiative to imp