Strengthening ethnicity data across the NHS: developing the national improvement plan
Our analysis and stakeholder engagement supported NHS England to develop the national Ethnicity Recording Improvement Plan.

A fairer funding future for general practice: lessons from Leicester, Leicestershire and Rutland ICB
Our evaluation of the Health Equity Payment (HEP) scheme in Leicester, Leicestershire and Rutland highlights how flexible, needs-based GP funding can support more equitable care.

A missing element in ‘shifting care’
Our Director, Peter Spilsbury, outlines the scale of the task when it comes to making ‘the shift from hospital to community’.

Hydration, UTIs and older people: learning from NHS pilots about how to improve care
Our evaluation of hydration-focused interventions for older people found promising signs of impact and highlighted the practical and systemic challenges of delivering and sustaining change.

Virtual wards: Patient and unpaid carer experiences of ‘hospital at home’ care
Our evaluation of patient and carer experiences of virtual wards found widespread benefits and highlights areas for improvements parti

“Champion, challenge, collaborate.”
Being commissioned by the Mayor of London to produce independent reviews of proposals for major service change, affecting Londoners, perfectly aligns with our commitment to help the health and care system make better decisions and ultimately achieve benefits for population health and wellbeing.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.
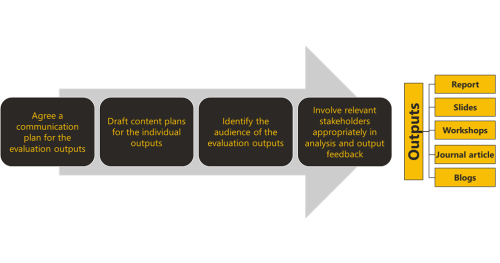
Our collective responsibility to share evaluation findings
The Strategy Unit is increasingly being commissioned to undertake evaluations on the pre
A Guide to Effective Evaluation: Design, Principles and Practice
Evaluation is key to making better decisions in health and care– understanding what works, for whom, and why.
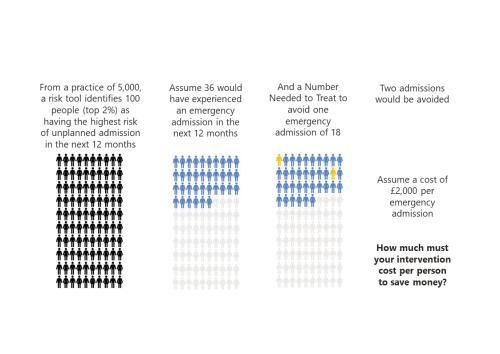
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.
Evaluating NHS England’s national approach to tackling healthcare inequalities
NHS England have commissioned the Strategy Unit to evaluate the national Core20PLUS5 approach for reducing healthcare inequalities.
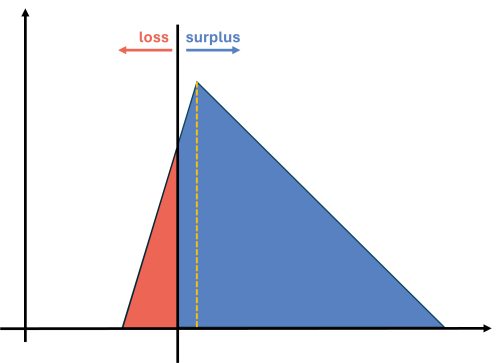
Contracting for health outcomes: from concept through theory to implementation
In this new report, jointly authored with colleagues from the University of York and The Royal Orthopaedic Hospital NHS Foundation Trust, we set out in detail how an outcomes-based contract for elective knee replacements might be constructed, and the potential implications for commissioners, providers, and policy-makers.
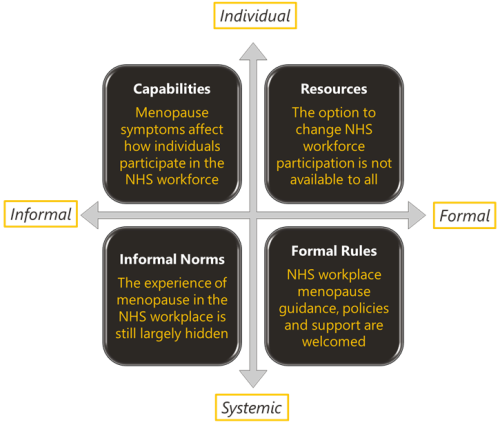
Menopause and the NHS workforce
The impact of the menopause on the NHS workforce. The Strategy Unit and Health Economics Unit report on their mixed methods findings.

Learning about what works in urgent community response
The initial report from the national urgent community response (UCR) evaluation, along with an economic modelling tool to help service providers and systems understand the impact of UCR, is now available.

Inclusive Elective Care Recovery
These case studies present the key features and learning from local initiatives which championed inclusive approaches to elective care recovery.

The NHS as an anchor institution: addressing fuel poverty
The number of households in fuel poverty in Staffordshire and Stoke-on-Trent (SSoT) is higher than the national average. As anchor institutions, NHS organisations can use their assets to influence the health and wellbeing of their local communities. The Strategy Unit was asked by the Midlands NHS Greening Board to evaluate a cross-sector initiative in SSoT to help alleviate fuel poverty using savings generated through solar panels on NHS buildings. The project is called Keep Warm, Keep Well.
MDSN: Evaluating Social Prescribing Literature Review
Evaluating Social Prescribing – Literature review for the MDSN Evaluation Community of Practice collaborative project

What are the ethical challenges in addressing inequities?
Produced by Angie Hobbs - the world’s first Professor in the Public Understanding of Philosophy – this paper examines the ethical questions raised by our report outlining strategies for reducing inequity.

Menopause and the NHS workforce
Now with the World Menopause Day 2022 update. What is it like to experience menopause as an NHS employee? And what is its impact on both the individuals and the organisations they work for?