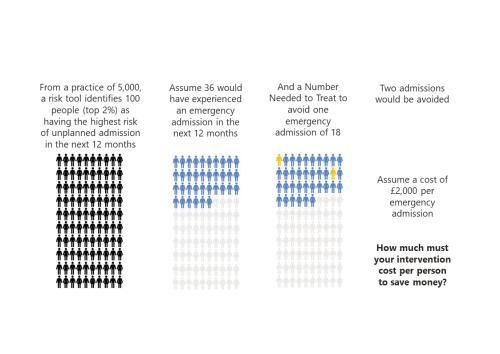
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.
MDSN: GP practice productivity, efficiency, and continuity of care
GP Practice productivity, efficiency, and continuity of care
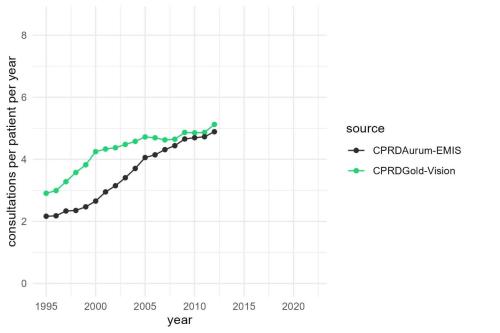
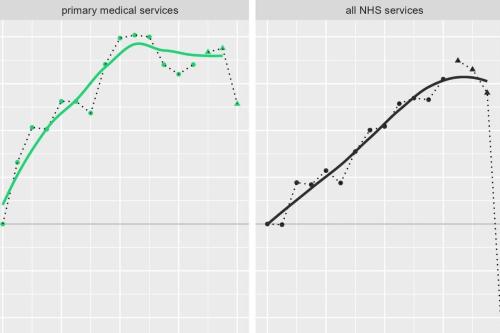
MDSN: Long-term trends in GP practice Consultation Rates
GP practice consultations are, by some distance, the most common interaction between the NHS and the population it serves.
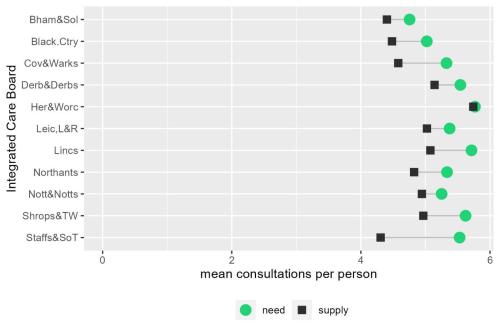
MDSN: The gap between need and supply of GP practice consultations
The gap between need and supply of GP practice consultations
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

Blog: Strategies to reduce inequalities in planned care
MDSN responds to recent reports addressing the NHS waiting list crisis
Strategies to reduce inequalities in access to planned hospital procedures
In our 2021 report, we described how people living in more deprived areas have poorer access to planned hospital care than their more affluent counterparts.

Advancing the analytical capability of the NHS and its ICS partners
The Strategy Unit were asked by the Strategy and Development Team in the Directorate of the Chief Data and Analytics Officer, NHSE/I, to make recommendations for advancing analytical capability across the health and care workforce.

Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.
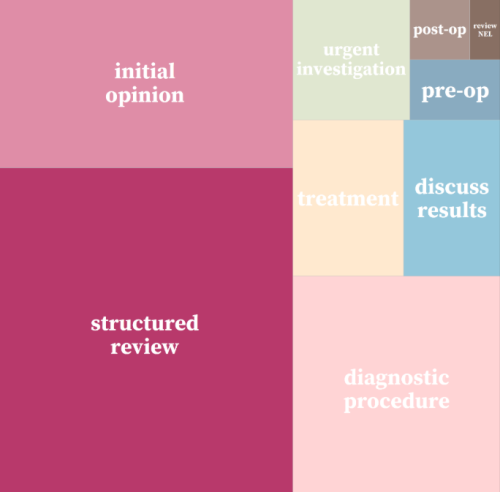
INSIGHT 2021: A new resource to support analysis of outpatient services
In this session, Andrew Jones presented a new classification system designed to enrich analyses of outpatient activity.

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
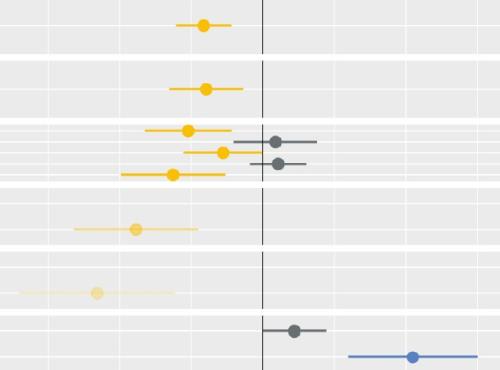
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
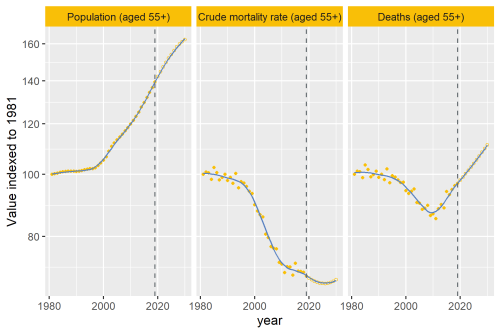
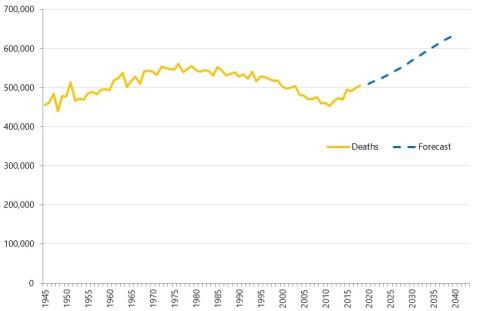
Why are deaths set to rise?
In our recent analysis of healthcare use in the last 2 years of life, we point out an important change that’s taking place to life and death in the UK.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.

Population Health Management Analyst Development Programme: An overview
The Population Health Management (PHM) Analyst Development Programme will introduce analysts from the Midlands CCGs, NHS Trusts, CSUs, Local Author
Waiting Times and Attendance Durations at English A&E Departments
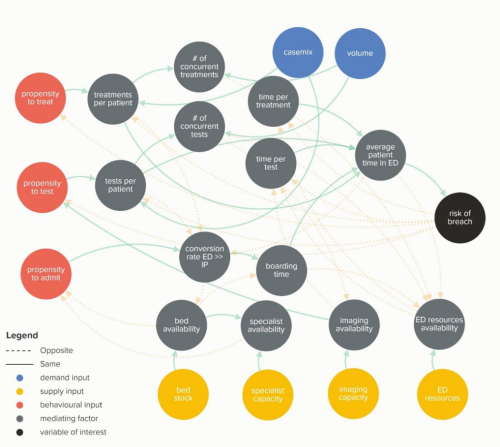
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.
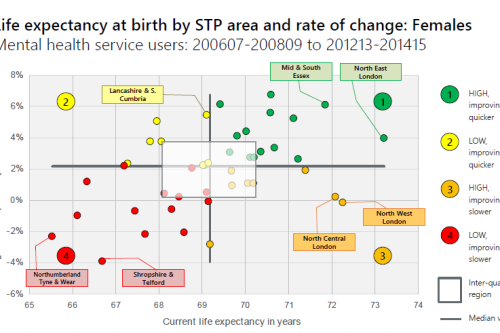
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20