
Strategy Unit releases opensource model for planning vaccine centre capacity
The UK is running its largest ever vaccination programme. The stakes are enormous.
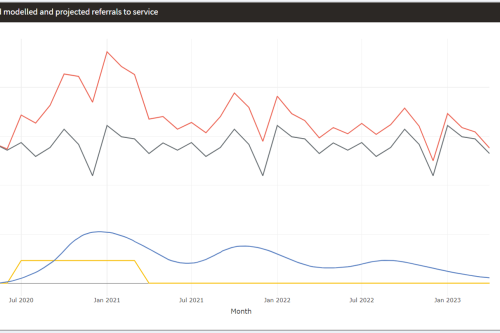
Mental Health Surge Model
Early in the Covid pandemic, it became clear that people’s mental health would suffer. Whether through bereavement, unemployment, social isolation, not being able to access support services – or a host of other routes – an alarming picture began to emerge and attract attention.
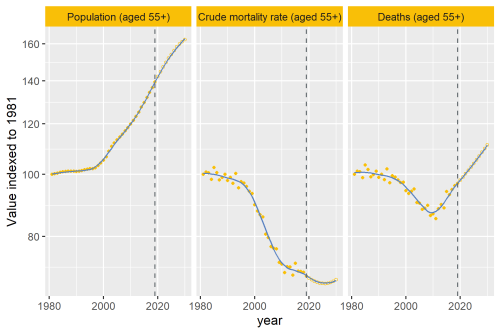
Why are deaths set to rise?
In our recent analysis of healthcare use in the last 2 years of life, we point out an important change that’s taking place to life and death in the UK.

Making sense of evidence
It's time to celebrate World Evidence-Based Healthcare (EBHC) Day. In a world dominated by COVID-19 and the associated infodemic, this day arguably has more resonance. Closer to home, EBHC Day also coincides with our Insight 2020 festival and the launch of the Midlands Decision Support network. What better opportunity to ask, 'what does evidence-informed decision making actually mean'?
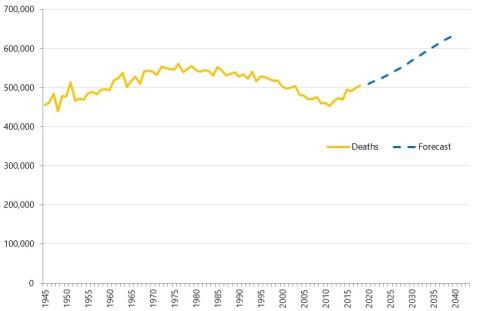
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.

Socio-economic and environmental impact of Herefordshire and Worcestershire STP
Anchor institutions are large, typically non-profit, public sector organisations whose long-term sustaina

Accessibility of perinatal mental health services for women from Ethnic Minority groups
Barriers to accessing mental health care during pregnancy and the first postnatal year (perinatal period) seem to be greater for ethnic minority women.
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.
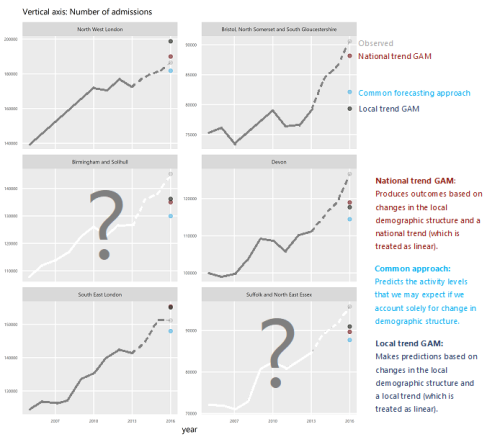
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.
Opening the ‘black box’ of scenario planning through realist synthesis
Scenario planning is recognised as an effective aid to strategic planning in complex, uncertain conditions. It is an approach that the Strategy Unit is increasingly building into its work with health and care systems and third sector organisations.
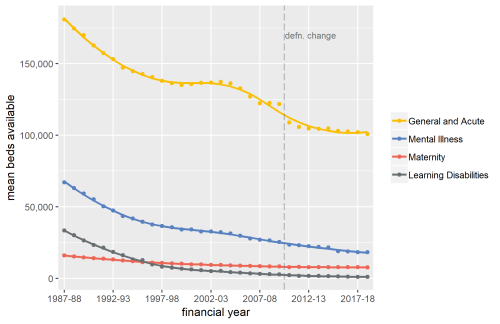
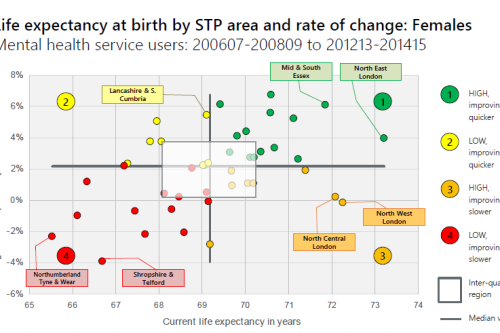
Exploring Mental Health Inpatient Capacity
This report explores the pressures on inpatient mental health services across Sustainability and Transformation Partnerships in England, drawing on a wide range of datasets, published research and interviews with staff working on mental health services. The report was commissioned by and includes a response from the Royal College of Psychiatrists.
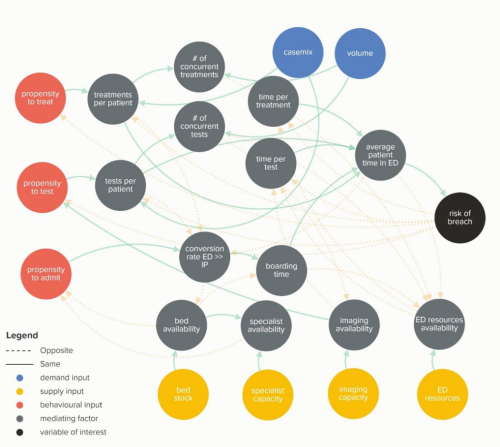
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.
New care models - what's the evidence
High level findings from a series of evidence reviews on new care models.
The Potential Economic Impact of Virtual Outpatient Appointments in the West Midlands: A scoping study
The Strategy Unit was recently approached to examine the case for a shift from traditional outpatient services to the use of virtual a
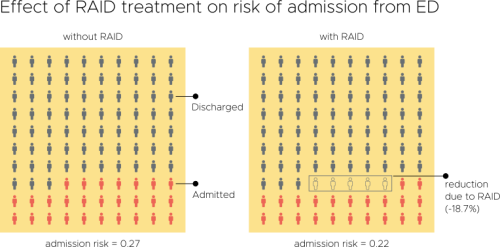
Evaluation of an Integrated Mental Health Liaison Service (Rapid Assessment Interface and Discharge Service) in Northern Ireland
A high proportion of patients treated for physical health conditions also have co-morbid mental health problems; and there is growing acceptance of
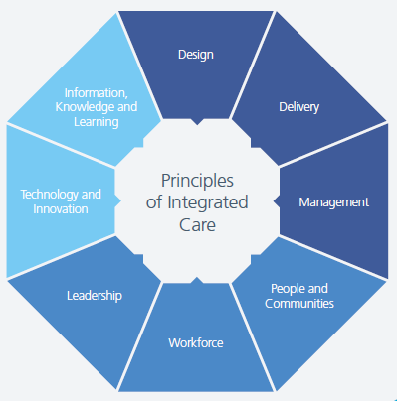
Integrating health and care services - what works? It’s complicated…
Coinciding nicely with the NHS 70th Birthday celebrations and the parallel discussions of ‘where next and how to do it better’ for the NHS, last we
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20
Risk and Reward Sharing for NHS Integrated Care Systems
Risk and reward sharing is a simple and attractive concept, offering a commissioner the opportunity to co-opt and incentivise a provid
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally integrate with a mental health trust, or set up a stand-alone community trust or Community Interest Company? Seven years on, this report explores the impact this choice had on the level and growth in emergency hospital use in older people and considers the wider implications for the NHS as it develops new models of care and integrated care systems

What works for primary care led integration?
We recently shared highlights from our realist synthesis on primary care-led integrated models, at the Health Policy and Planning Network workshop. Take a look at our presentation for a flavour of our findings ahead of publication later in the summer.