
Beating the backlog: Meeting the waiting list challenge
The NHS waiting list in England must halve to reach waiting time targets.
Strategy Unit demand model wins prestigious Florence Nightingale Award
Our open-source demand model, developed in collaboration with the New Hospital Programme, has been named the 2025 winner of the Florence Nightingale Award for Excellence in Health and Care Analytics.
Transforming Hospital Planning with an Open-Source Demand and Capacity Model
We are proud to announce the open-sourcing of a demand and capacity model, developed with the New Hospitals Programme, to transform NHS hospital planning with transparency, collaboration, and efficiency.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
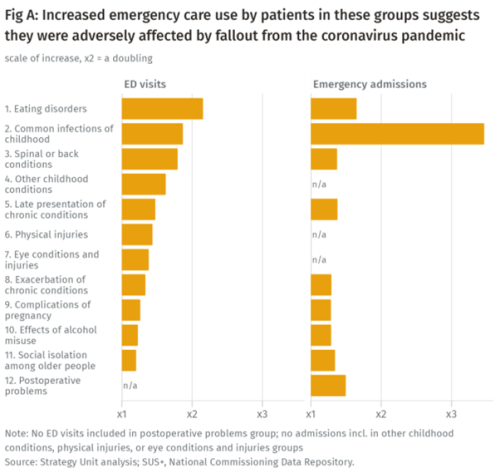
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.

Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
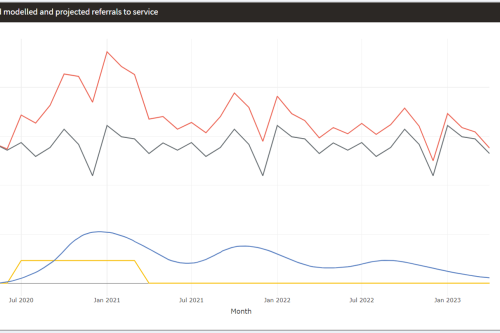
Mental Health Surge Model
Early in the Covid pandemic, it became clear that people’s mental health would suffer. Whether through bereavement, unemployment, social isolation, not being able to access support services – or a host of other routes – an alarming picture began to emerge and attract attention.
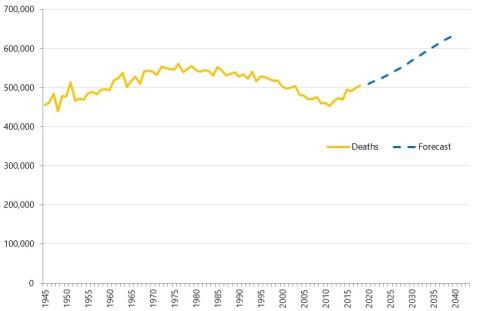
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.

Accessibility of perinatal mental health services for women from Ethnic Minority groups
Barriers to accessing mental health care during pregnancy and the first postnatal year (perinatal period) seem to be greater for ethnic minority women.
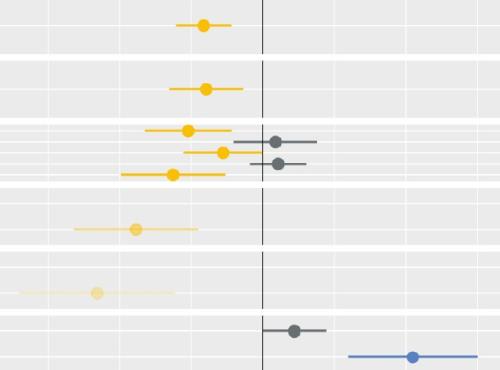
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.
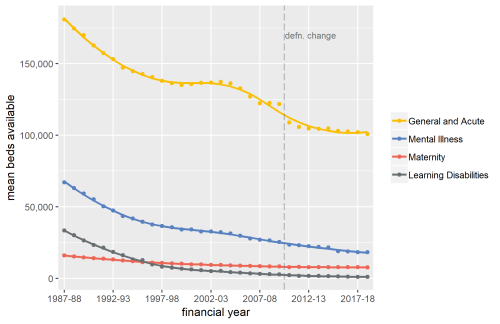
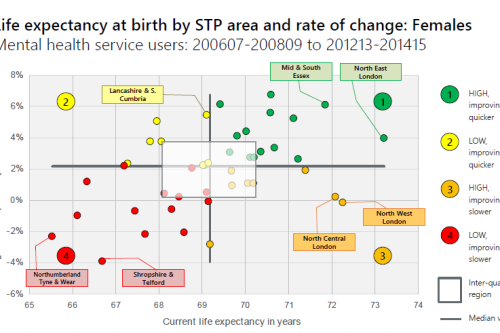
Exploring Mental Health Inpatient Capacity
This report explores the pressures on inpatient mental health services across Sustainability and Transformation Partnerships in England, drawing on a wide range of datasets, published research and interviews with staff working on mental health services. The report was commissioned by and includes a response from the Royal College of Psychiatrists.
The Potential Economic Impact of Virtual Outpatient Appointments in the West Midlands: A scoping study
The Strategy Unit was recently approached to examine the case for a shift from traditional outpatient services to the use of virtual a
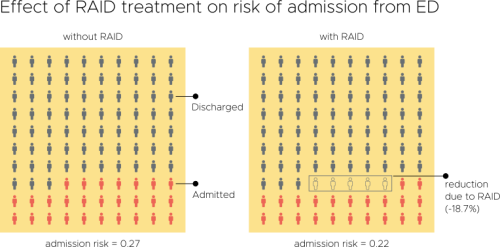
Evaluation of an Integrated Mental Health Liaison Service (Rapid Assessment Interface and Discharge Service) in Northern Ireland
A high proportion of patients treated for physical health conditions also have co-morbid mental health problems; and there is growing acceptance of
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20
Changes in Dementia Incidence, Prevalence, Severity and Mortality
Dementia is a key priority for NHS England and is estimated to affect around 676,000 people in the country.
Making the Case for Integrating Mental and Physical Health Care - Full Report.
An analysis of the physical health of people who use mental health services: life expectancy, acute service use and the potential for