
A fairer funding future for general practice: lessons from Leicester, Leicestershire and Rutland ICB
Our evaluation of the Health Equity Payment (HEP) scheme in Leicester, Leicestershire and Rutland highlights how flexible, needs-based GP funding can support more equitable care.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘Internal Consultancy’: INSIGHTS from evidence and experience
In this blog, our Head of Policy, Fraser Battye, shares his reflections on a recent ‘SU INSIGHTS’ event on the ‘Internal Consultancy’

From ‘right drift’ to ‘left shift’?
Our Head of Policy, Fraser Battye, looks at the challenges facing the intention to shift care ‘from hospital to community’. He suggests that we have missed a critical part of the explanation for why this ‘left shift’ hasn’t taken place following previous initiatives.
Evaluating NHS England’s national approach to tackling healthcare inequalities
NHS England have commissioned the Strategy Unit to evaluate the national Core20PLUS5 approach for reducing healthcare inequalities.

What are the downsides of digital?
What are the downsides of digital?

The risks of risk stratification
Medical history is full of bizarre and gruesome procedures.

Want to ease pressure in urgent care? Simply cut community services!?!
What should decision makers do with analysis that challenges deeply held assumptions? In this blog, Fraser Battye reflects on a surprising recent finding about community services.
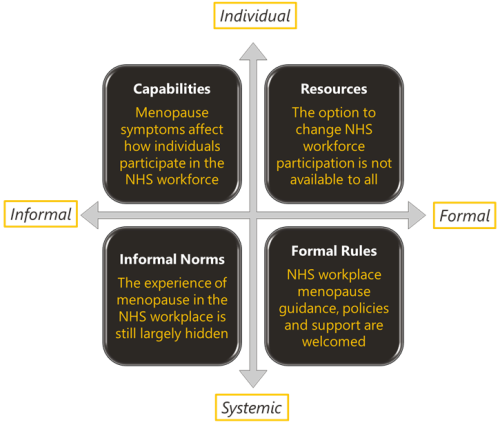
Menopause and the NHS workforce
The impact of the menopause on the NHS workforce. The Strategy Unit and Health Economics Unit report on their mixed methods findings.

Learning about what works in urgent community response
The initial report from the national urgent community response (UCR) evaluation, along with an economic modelling tool to help service providers and systems understand the impact of UCR, is now available.

Inclusive Elective Care Recovery
These case studies present the key features and learning from local initiatives which championed inclusive approaches to elective care recovery.

The NHS as an anchor institution: addressing fuel poverty
The number of households in fuel poverty in Staffordshire and Stoke-on-Trent (SSoT) is higher than the national average. As anchor institutions, NHS organisations can use their assets to influence the health and wellbeing of their local communities. The Strategy Unit was asked by the Midlands NHS Greening Board to evaluate a cross-sector initiative in SSoT to help alleviate fuel poverty using savings generated through solar panels on NHS buildings. The project is called Keep Warm, Keep Well.
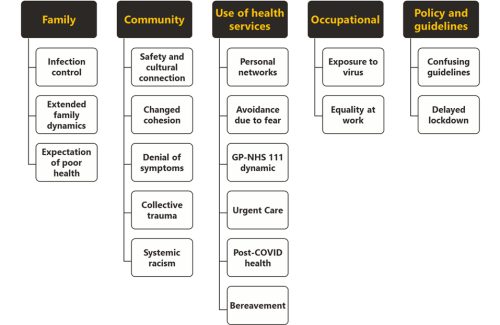
We don’t just need to hear ‘you are more affected’ - what’s the action?
The experience of minority ethnic people symptomatic for COVID-19 in the first UK wave of the pandemic.

Evaluation of Building the Right Support: Final Reports
Building the Right Support was a national plan to provide better support to people with a learning disability or autism.

Inequities in children and young people’s mental health services
Good mental health during early years and childhood has a great bearing on health throughout life.

Increasing vaccine uptake
The purpose of this work was to identify the key features of local initiatives which encourage vaccine uptake in different population groups, and share these for others to learn from.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of

Learning from lockdown: support for people experiencing homelessness
There are few clearer measures of societal health than homelessness.
How can Integrated Care Systems collect and use more ‘person-centred intelligence’?
Working with our partners
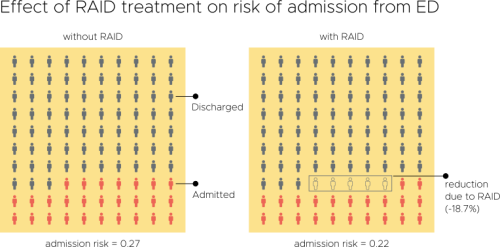
Evaluation of an Integrated Mental Health Liaison Service (Rapid Assessment Interface and Discharge Service) in Northern Ireland
A high proportion of patients treated for physical health conditions also have co-morbid mental health problems; and there is growing acceptance of