
Planning for rising renal demand: simulating capacity across the care system
Demand for kidney replacement therapy is rising, and current capacity will not be sufficient over the next decade. This work uses simulation modelling to help systems understand future pressures and test potential responses.

Death (and taxes?)
Hospices are fundamental to end of life care, and the broader shift ‘from hospital to community’.

Beating the backlog: Meeting the waiting list challenge
The NHS waiting list in England must halve to reach waiting time targets.

Cancer and comorbidities: An Evidence Review of Diagnosis, Treatment, and Experience
An evidence review on the challenges and disparities faced by individuals living with cancer alongside other long-term conditions.
Strategy Unit demand model wins prestigious Florence Nightingale Award
Our open-source demand model, developed in collaboration with the New Hospital Programme, has been named the 2025 winner of the Florence Nightingale Award for Excellence in Health and Care Analytics.

Virtual wards: Patient and unpaid carer experiences of ‘hospital at home’ care
Our evaluation of patient and carer experiences of virtual wards found widespread benefits and highlights areas for improvements parti
Transforming Hospital Planning with an Open-Source Demand and Capacity Model
We are proud to announce the open-sourcing of a demand and capacity model, developed with the New Hospitals Programme, to transform NHS hospital planning with transparency, collaboration, and efficiency.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘Internal Consultancy’: INSIGHTS from evidence and experience
In this blog, our Head of Policy, Fraser Battye, shares his reflections on a recent ‘SU INSIGHTS’ event on the ‘Internal Consultancy’

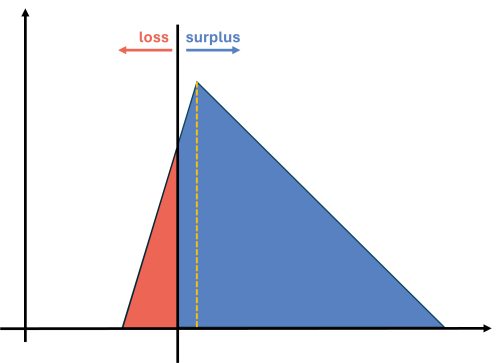
From ‘right drift’ to ‘left shift’?
Our Head of Policy, Fraser Battye, looks at the challenges facing the intention to shift care ‘from hospital to community’. He suggests that we have missed a critical part of the explanation for why this ‘left shift’ hasn’t taken place following previous initiatives.

Charisma
In this long read, which first appeared in the HSJ, Fraser Battye - our Head of Policy – looks at the role of charisma and innovation in the way that NHS resources are allocated.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.

Ara Darzi, Wes Streeting and English health policy. Part 2: cutting the knot
Following on from part one, Fraser continues exploring the Gordian Knot of English health policy.

Ara Darzi, Wes Streeting and English health policy. Part 1: the Gordian Knot
Health policy is not at a crossroads, it is in a bind. Strands so entangled, so complex they resemble a Gordian knot. Can this knot be untied?

Want to ease pressure in urgent care? Simply cut community services!?!
What should decision makers do with analysis that challenges deeply held assumptions? In this blog, Fraser Battye reflects on a surprising recent finding about community services.
Contracting for health outcomes: from concept through theory to implementation
In this new report, jointly authored with colleagues from the University of York and The Royal Orthopaedic Hospital NHS Foundation Trust, we set out in detail how an outcomes-based contract for elective knee replacements might be constructed, and the potential implications for commissioners, providers, and policy-makers.

Playing our part in conversations about death
“Dad, why are all your ‘peptalks’ about death?” Children can be a source of fundamental insight. They seem to specialise in feedback of the unvarnished, unmediated and fully caffeinated variety. The kind of feedback that cuts straight to it. My youngest daughter, mid-way through our sunny walk down the hill to school, pressed on: “And you wear black all the time. You look like a crow…” Fundamental insight, and now fashion advice. This was quite the school run.

A Picture of End-of-Life Care in England
Working with Macmillan our analysis investigates who is more likely to experience poor outcomes associated with shortcomings in end-of-life care? Are there particular areas in England where those at end-of-life face significant challenges and how might the supply of services in an area be influencing these?

Review of Ophthalmic Managed Clinical Networks (MCNs) in Staffordshire and Shropshire
The aim of the MCNs is to bring together primary care optometrists with local ophthalmologists within a geographical area. This is a review Strategy Unit were commissioned by NHS England to work with a medical retina MCN in Shropshire, Telford and Wrekin and a glaucoma MCN in Staffordshire and Stoke on Trent, to review their work so far and look at the opportunities the networks present.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.