Contracting for health outcomes: from concept through theory to implementation
In this new report, jointly authored with colleagues from the University of York and The Royal Orthopaedic Hospital NHS Foundation Trust, we set out in detail how an outcomes-based contract for elective knee replacements might be constructed, and the potential implications for commissioners, providers, and policy-makers.

Part-time GPs and the decline in continuity of care: a cause or a symptom?
In our recent paper we explore why levels of care continuity have been declining and what might be done to turn things around.

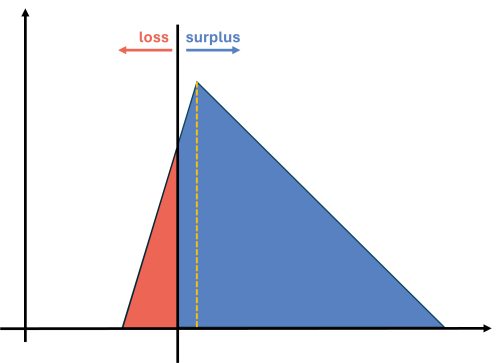
Two sides of the same coin
Hospital demand arising from GPs not seeing patients, is eating into the resources that they would use to manage down the elective backlog. In turn, this is creating more demand for GPs.

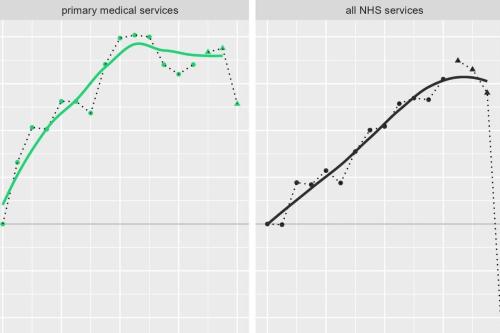
Are GP consultation rates rising or falling? Who or what should we believe?
If the "data suggests" GP appointments are substantially higher than pre-pandemic, then what is behind patients reporting recieving fewer appointments?

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.
MDSN: GP practice productivity, efficiency, and continuity of care
GP Practice productivity, efficiency, and continuity of care
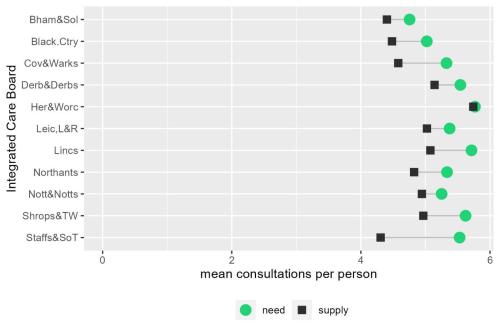
MDSN: The gap between need and supply of GP practice consultations
The gap between need and supply of GP practice consultations
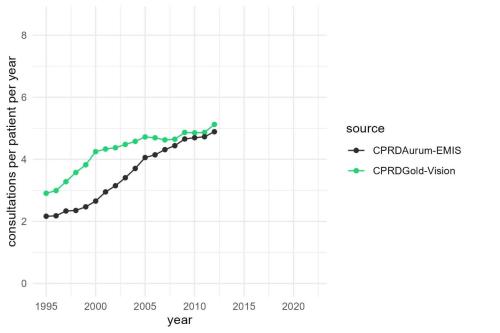
MDSN: Long-term trends in GP practice Consultation Rates
GP practice consultations are, by some distance, the most common interaction between the NHS and the population it serves.
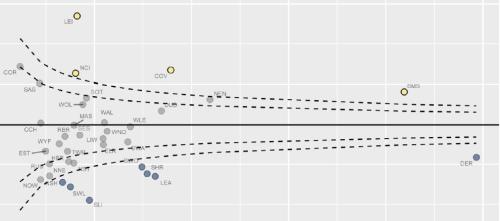
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

Strategies to reduce inequalities in access to planned hospital procedures
UPDATE 10th August: Now including briefing note for Integrated Care Boards on legal duties in respect of reducing inequalities. This report guides ICBs through the process.

Securing the future of domiciliary care
The Strategy Unit is embarking on an exciting project with WM ADASS, the Association of Directors of Adult Social Care Services in the West Midlands to explore the challenges facing domiciliary care and the opportunities that exist to transform and improve the service.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
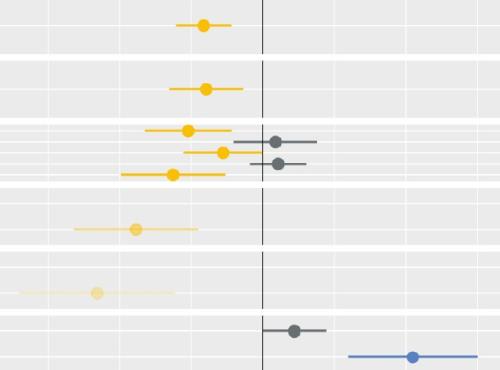
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions.
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally integrate with a mental health trust, or set up a stand-alone community trust or Community Interest Company? Seven years on, this report explores the impact this choice had on the level and growth in emergency hospital use in older people and considers the wider implications for the NHS as it develops new models of care and integrated care systems
Making the Case for Integrating Mental and Physical Health Care - Full Report.
An analysis of the physical health of people who use mental health services: life expectancy, acute service use and the potential for
