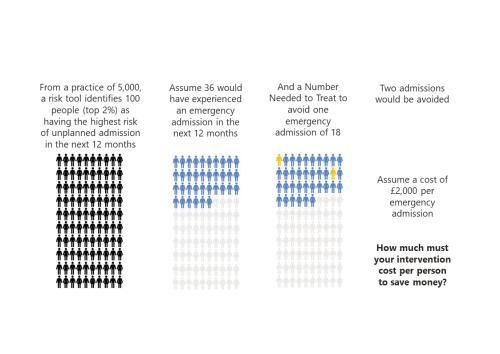
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.

Part-time GPs and the decline in continuity of care: a cause or a symptom?
In our recent paper we explore why levels of care continuity have been declining and what might be done to turn things around.

Two sides of the same coin
Hospital demand arising from GPs not seeing patients, is eating into the resources that they would use to manage down the elective backlog. In turn, this is creating more demand for GPs.

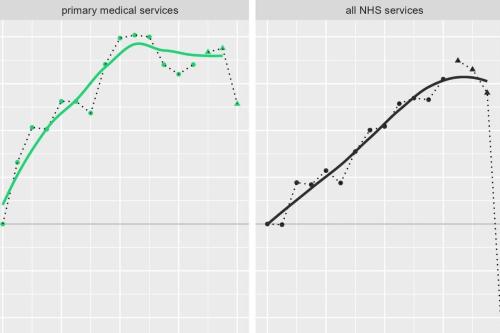
Are GP consultation rates rising or falling? Who or what should we believe?
If the "data suggests" GP appointments are substantially higher than pre-pandemic, then what is behind patients reporting recieving fewer appointments?

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.
MDSN: GP practice productivity, efficiency, and continuity of care
GP Practice productivity, efficiency, and continuity of care
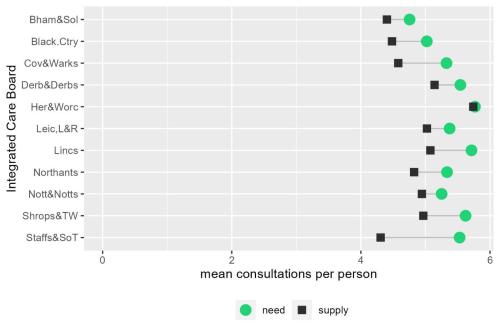
MDSN: The gap between need and supply of GP practice consultations
The gap between need and supply of GP practice consultations
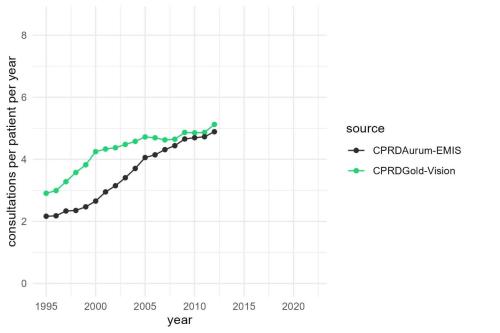
MDSN: Long-term trends in GP practice Consultation Rates
GP practice consultations are, by some distance, the most common interaction between the NHS and the population it serves.
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

Advancing the analytical capability of the NHS and its ICS partners
The Strategy Unit were asked by the Strategy and Development Team in the Directorate of the Chief Data and Analytics Officer, NHSE/I, to make recommendations for advancing analytical capability across the health and care workforce.

Securing the future of domiciliary care
The Strategy Unit is embarking on an exciting project with WM ADASS, the Association of Directors of Adult Social Care Services in the West Midlands to explore the challenges facing domiciliary care and the opportunities that exist to transform and improve the service.

Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of
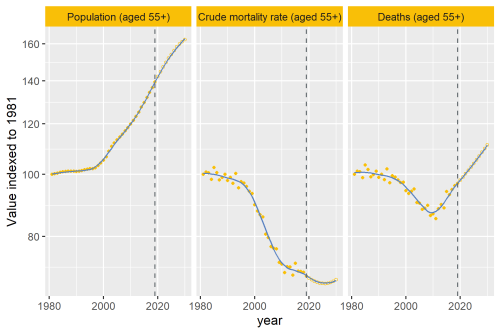
Why are deaths set to rise?
In our recent analysis of healthcare use in the last 2 years of life, we point out an important change that’s taking place to life and death in the UK.
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.
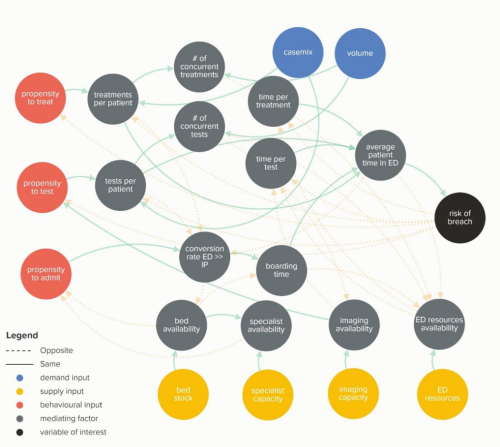
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.