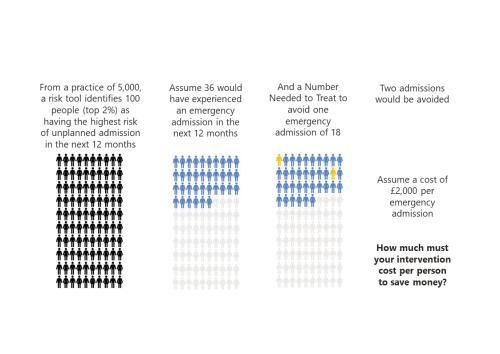
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

Advancing the analytical capability of the NHS and its ICS partners
The Strategy Unit were asked by the Strategy and Development Team in the Directorate of the Chief Data and Analytics Officer, NHSE/I, to make recommendations for advancing analytical capability across the health and care workforce.

Estimating the impact of the proposed reforms to the Mental Health Act on the workload of psychiatrists
In January 2021, the Government published a White Paper, setting out its plans to reform the Mental Health Act.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department

Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
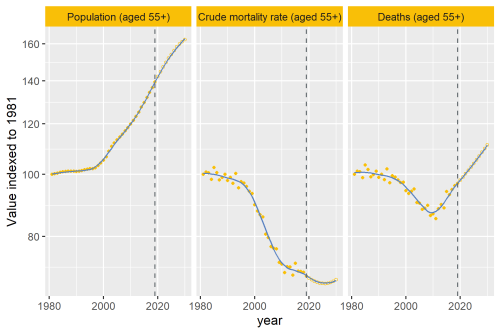
Why are deaths set to rise?
In our recent analysis of healthcare use in the last 2 years of life, we point out an important change that’s taking place to life and death in the UK.
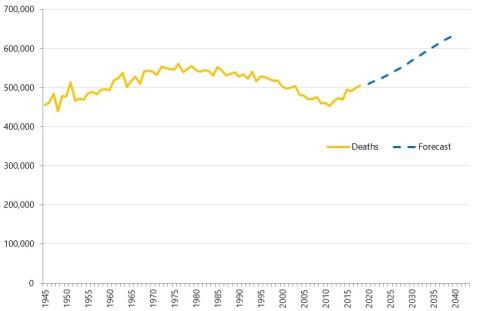
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike Woodall explain what we did and how we did it.
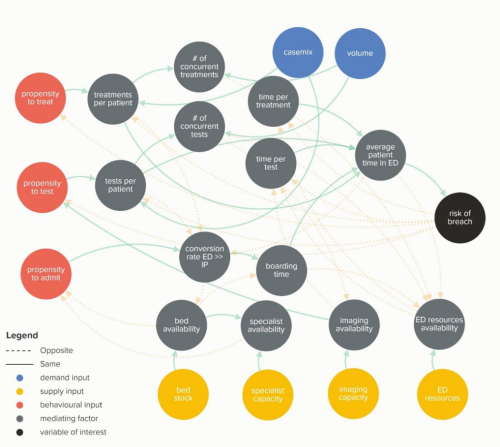
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.
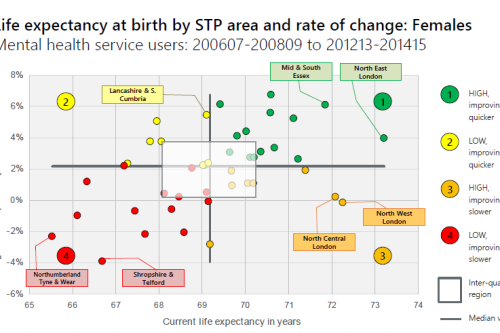
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20
Risk and Reward Sharing for NHS Integrated Care Systems
Risk and reward sharing is a simple and attractive concept, offering a commissioner the opportunity to co-opt and incentivise a provid
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally integrate with a mental health trust, or set up a stand-alone community trust or Community Interest Company? Seven years on, this report explores the impact this choice had on the level and growth in emergency hospital use in older people and considers the wider implications for the NHS as it develops new models of care and integrated care systems