
Mending smarter, not harder: Changing fracture care for children
The report demonstrates there is significant variation between trusts in England in how paediatric fractures are managed. Widespread adoption of less interventional approaches to paediatric fracture management could result in significant savings in hospital activity, particularly reduced follow-up appointments for uncomplicated fractures.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department

Inequities in children and young people’s mental health services
Good mental health during early years and childhood has a great bearing on health throughout life.

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.

Accessibility of perinatal mental health services for women from Ethnic Minority groups
Barriers to accessing mental health care during pregnancy and the first postnatal year (perinatal period) seem to be greater for ethnic minority women.
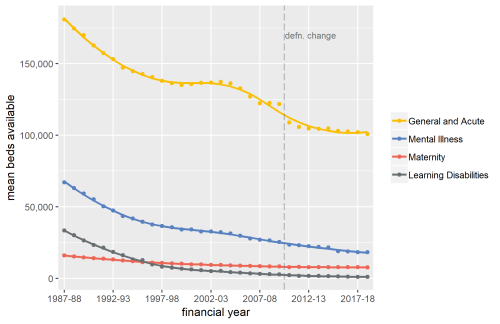
Exploring Mental Health Inpatient Capacity
This report explores the pressures on inpatient mental health services across Sustainability and Transformation Partnerships in England, drawing on a wide range of datasets, published research and interviews with staff working on mental health services. The report was commissioned by and includes a response from the Royal College of Psychiatrists.

They don’t believe you
Continuing our mental and physical health guest blog series, Sophie Corlett the Director of External Relations at Mind provides some perspectives from people with physical ailments who are users of mental health services.

Mind and body: inseparable twins
Jennifer Dixon, Chief Executive of the Health Foundation, reflects on the relationship between mental and physical health and the need for better integration of care.

Warp and weft – recognising that physical and mental health are interwoven - By Professor Sir Muir Gray
On World Mental Health Day, we’re delighted to present a guest blog by Professor Sir Muir Gray, the first in a new series of commi
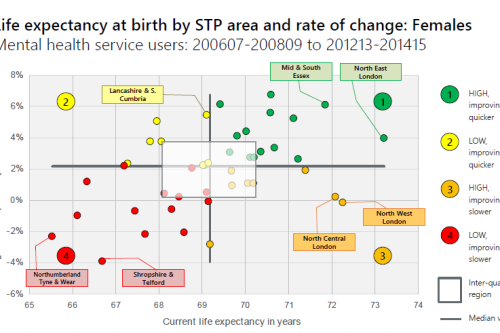
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 20
Mental Health and integration: Cinderella or the Ugly Sisters?
Introduction
Do you like to integrate horizontally or vertically? NHS positions examined
Our latest research paper explores the impact of the different options for integration implemented as a result of the Transforming Community Services policy in 2010. This accompanying commentary reflects on potential implications for the current policy drive towards Integrated Care Systems.
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally integrate with a mental health trust, or set up a stand-alone community trust or Community Interest Company? Seven years on, this report explores the impact this choice had on the level and growth in emergency hospital use in older people and considers the wider implications for the NHS as it develops new models of care and integrated care systems
Making the Case for Integrating Mental and Physical Health Care - Full Report.
An analysis of the physical health of people who use mental health services: life expectancy, acute service use and the potential for

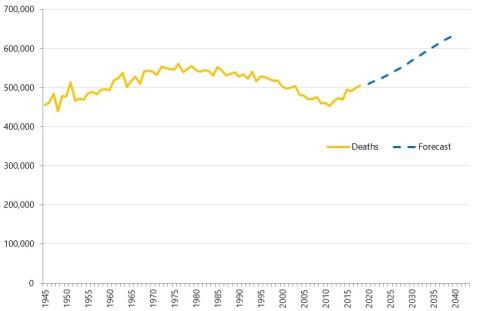
The Effect of Demographic Change on Acute Hospital Utilisation
Recognising that the effect of population ageing can be overstated, we set out to ask what effect an older population will have on demand for
Identifying Potential QIPP Opportunities - Dudley Example
Given the pressures within the NHS, being able to identify opportunities for efficiencies and improvements is