
Inclusive Elective Care Recovery
These case studies present the key features and learning from local initiatives which championed inclusive approaches to elective care recovery.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

The NHS as an anchor institution: addressing fuel poverty
The number of households in fuel poverty in Staffordshire and Stoke-on-Trent (SSoT) is higher than the national average. As anchor institutions, NHS organisations can use their assets to influence the health and wellbeing of their local communities. The Strategy Unit was asked by the Midlands NHS Greening Board to evaluate a cross-sector initiative in SSoT to help alleviate fuel poverty using savings generated through solar panels on NHS buildings. The project is called Keep Warm, Keep Well.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).
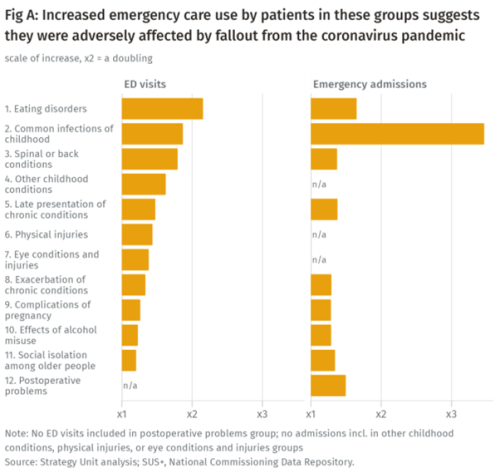
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.
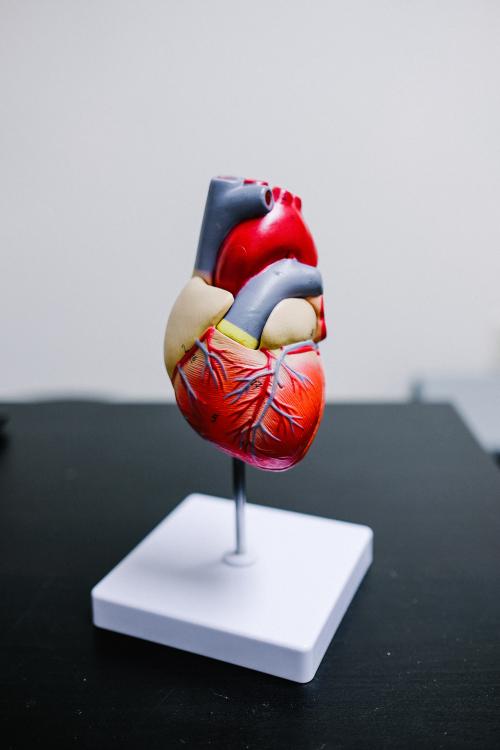
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified

Helping ICSs to reduce inequalities in access to planned care
Are there inequalities in access to planned care? If so, what are they? Which groups ‘gain’ and which groups suffer? And what could be done to address any inequalities? In pursuing their objective of reducing inequalities, what could Integrated Care Systems (ICSs) do? What strategies and approaches are likely to be successful?

What matters when waiting? – involving the public in NHS waiting list prioritisation
As the NHS emerged out of the pandemic, it was confronted with the challenge of not only recovery of unprecedented waiting lists, but with inequalities which required attention. NHS leaders challenged providers to restore inclusively and at University Hospitals Coventry and Warwickshire NHS Trust, we have developed a way of doing just that, whilst simultaneously reducing waiting times for all.

Inequalities in access to healthcare - what’s our next move?
Our research, published in the Lancet Regional Health Europe, highlights substantial inequities in access to elective hip replacement surgery. We found no evidence that these inequities reduced between 2006 and 2016.

Urgent Community Response – What Works?
The Strategy Unit, with our partners Ipsos, has been commissioned by NHS England and NHS Improvement (NHSEI) to provide a long-term national evaluation of the Urgent Community Response programme rolled-out across England. The programme aims to shift resources to home and community-based services as part of the NHS commitment to providing the right care, to the right people, at the right time. And there are a range of outputs from the early work that provide learning for local systems as they develop their services.

Strategies to reduce inequalities in access to planned hospital procedures
UPDATE 10th August: Now including briefing note for Integrated Care Boards on legal duties in respect of reducing inequalities. This report guides ICBs through the process.

Treating people on waiting lists: who decides what is fair?
Waiting lists for elective care are in the news. The national plan has been issued, with the expectation that lists will continue to rise for some years - and that long waiting will not disappear anytime soon. Addressing this ‘backlog’ will remain a fundamental challenge for some time to come.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.

Decisions to admit patients are not solely determined by clinical risk
Whether or not to admit a patient is one of the most routine yet important decisions a doctor in an Emergency Department
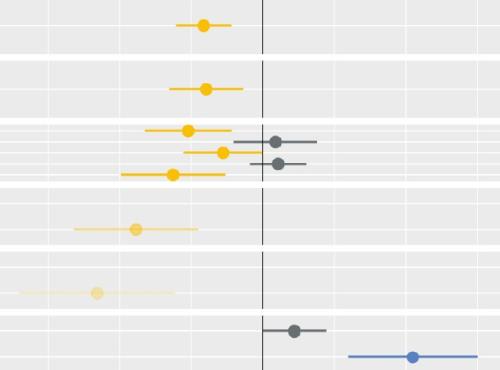
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.

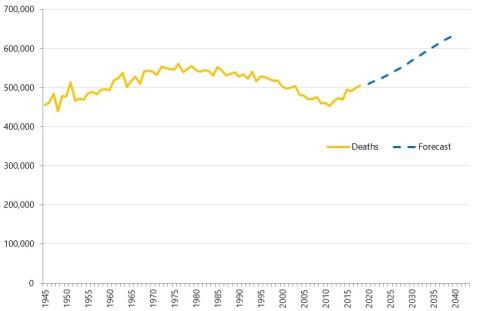
Evidence review: Early diagnosis of cancer
Detecting cancers early is essential to saving lives and reducing the need for invasive treatments.

Some positive news for integrating GP practices with hospital trusts
The drive for greater integration of health and care services has been the central theme of UK health policy for most of

Strategy Unit analysis published showing changes in use of emergency departments under lockdown
We know that patterns of access to healthcare have changed during the pandemic.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.