
Mending smarter, not harder: Changing fracture care for children
The report demonstrates there is significant variation between trusts in England in how paediatric fractures are managed. Widespread adoption of less interventional approaches to paediatric fracture management could result in significant savings in hospital activity, particularly reduced follow-up appointments for uncomplicated fractures.
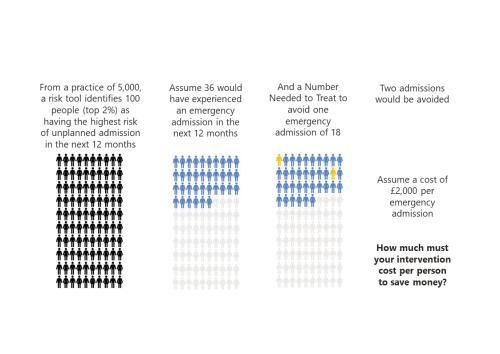
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.

MDSN: Community Healthcare Services
How Does Access to Community Health Services Vary Across the Midlands?

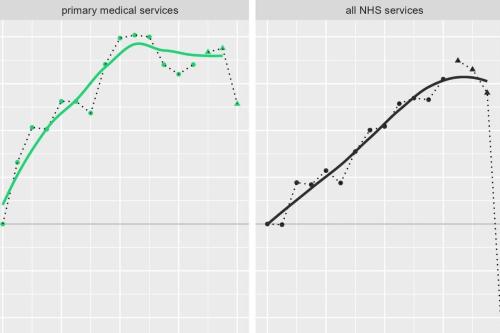
GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.
MDSN: GP practice productivity, efficiency, and continuity of care
GP Practice productivity, efficiency, and continuity of care
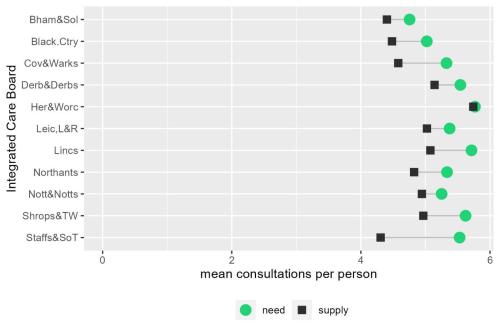
MDSN: The gap between need and supply of GP practice consultations
The gap between need and supply of GP practice consultations
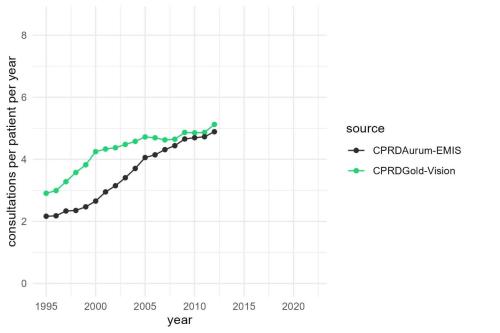
MDSN: Long-term trends in GP practice Consultation Rates
GP practice consultations are, by some distance, the most common interaction between the NHS and the population it serves.

Learning about what works in urgent community response
The initial report from the national urgent community response (UCR) evaluation, along with an economic modelling tool to help service providers and systems understand the impact of UCR, is now available.
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.

The NHS as an anchor institution: addressing fuel poverty
The number of households in fuel poverty in Staffordshire and Stoke-on-Trent (SSoT) is higher than the national average. As anchor institutions, NHS organisations can use their assets to influence the health and wellbeing of their local communities. The Strategy Unit was asked by the Midlands NHS Greening Board to evaluate a cross-sector initiative in SSoT to help alleviate fuel poverty using savings generated through solar panels on NHS buildings. The project is called Keep Warm, Keep Well.

Emergency department acuity measurement and process: quick scoping review
This review was commissioned to inform NHS England’s Acuity Standardisation Project which aims to agree a standardised method of allocating acuity category (a triage method) for Emergency Departments (EDs) and Urgent Treatment Centres (UTCs).
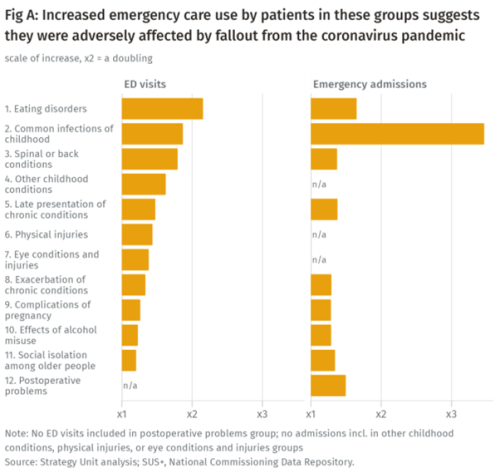
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.
Strategies to reduce inequalities in access to planned hospital procedures
In our 2021 report, we described how people living in more deprived areas have poorer access to planned hospital care than their more affluent counterparts.

Inequities in children and young people’s mental health services
Good mental health during early years and childhood has a great bearing on health throughout life.
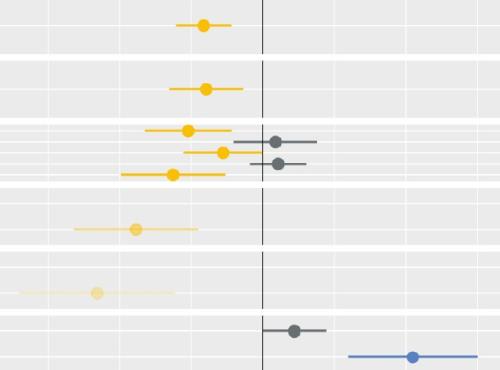
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
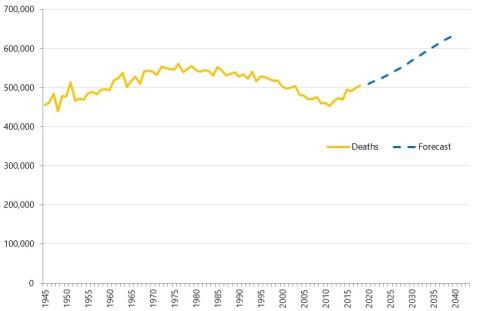
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.

Midlands Population Health Management Academy
The Midlands Population Health Management Academy was part of a programme of support, commissioned by NHS
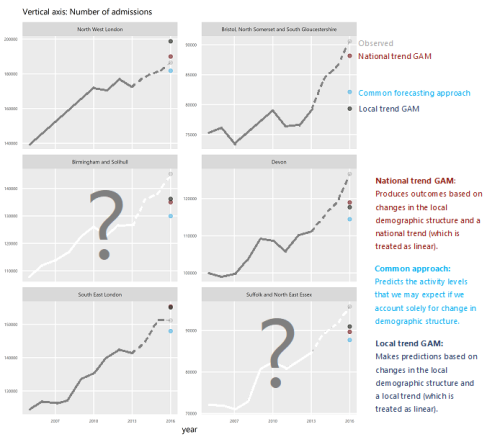
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.
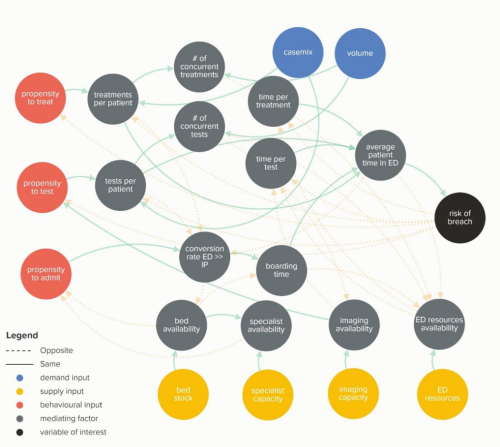
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis uncovers new insights and has the potential to reshape received wisdom about the performance of A&E departments, carrying important implications for healthcare policy and system leadership.
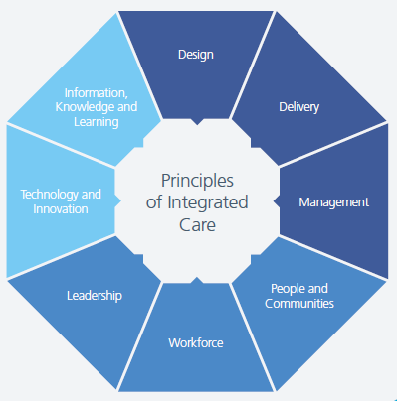
New care models - what's the evidence
High level findings from a series of evidence reviews on new care models.