 Better use of analysis | Elective care | Policy
Better use of analysis | Elective care | Policy
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
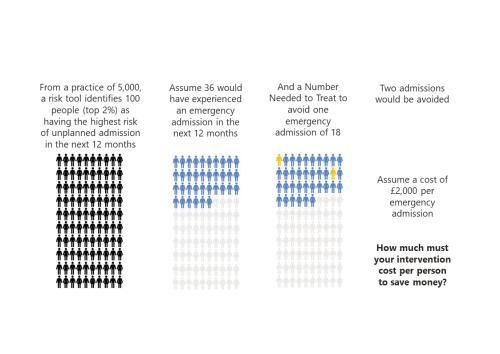
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive. By predicting the risk of future adverse events, we should be able to target efforts to avoid/mitigate them. Doing so would save both money and misery. But, as Niels Bohr said wryly, “Prediction isn’…
 Better use of analysis | Elective care | Inequalities
Better use of analysis | Elective care | Inequalities
Inclusive Elective Care Recovery
These case studies present the key features and learning from local initiatives which championed inclusive approaches to elective care recovery.
 Elective care | Emergency care | Policy
Elective care | Emergency care | Policy
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive…
 Inequalities | Public health and prevention | Secondary care
Inequalities | Public health and prevention | Secondary care
Socio-economic inequalities in coronary heart disease
There are substantial differences in mortality rates from cardiovascular disease between socio-economic groups. Our new tool provides an overview, for ICBs, of the points on the care pathway where inequalities emerge and are amplified
 Elective care | Inequalities | Policy
Elective care | Inequalities | Policy
What are the ethical challenges in addressing inequities?
Produced by Angie Hobbs - the world’s first Professor in the Public Understanding of Philosophy – this paper examines the ethical questions raised by our report outlining strategies for reducing inequity.
 Inequalities | Policy | Public health and prevention
Inequalities | Policy | Public health and prevention
Measuring the effect of the coronavirus pandemic on population health
Measuring the effect of the coronavirus pandemic on population health One feature of the pandemic has been the fast-flowing stream of facts and numbers about the impact of Covid-19. At the same time, we’ve had to absorb the meaning of terms that were previously the preserve of epidemiologists and…
 Better use of analysis | Elective care | Emergency care | Inequalities | Primary, community and social care services | Public health and prevention
Better use of analysis | Elective care | Emergency care | Inequalities | Primary, community and social care services | Public health and prevention
Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
 Policy | Primary, community and social care services | Public health and prevention
Policy | Primary, community and social care services | Public health and prevention
Increasing vaccine uptake
The purpose of this work was to identify the key features of local initiatives which encourage vaccine uptake in different population groups, and share these for others to learn from.
 Elective care | Inequalities | Policy | Primary, community and social care services
Elective care | Inequalities | Policy | Primary, community and social care services
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
 Inequalities | Policy | Primary, community and social care services | Public health and prevention
Inequalities | Policy | Primary, community and social care services | Public health and prevention
Reviewing the evidence on digital inclusion
Digital technology is a significant part of our daily lives. It has changed the way we interact with each other, the services we use, and the ways we work. The NHS is no exception. Digital technology has begun to change the way health…
 Elective care | Policy | Primary, community and social care services | Public health and prevention
Elective care | Policy | Primary, community and social care services | Public health and prevention
Evidence review: Early diagnosis of cancer
Detecting cancers early is essential to saving lives and reducing the need for invasive treatments. So, in 2019, the NHS Long Term Plan set a national target for increasing the proportion of cancers diagnosed at an early stage. There is room for improvement in current performance. In 2018, 55% of…
Strategy Unit analysis of air quality highlights inequalities
Poor air quality is the largest environmental risk to public health in the UK and central London has the highest levels of particulate matter and nitrogen dioxide. The Guy’s and St. Thomas’ charity, now operating its programmes under the Impact on Urban Health banner, have…
 Inequalities | Mental health | Policy | Primary, community and social care services | Public health and prevention
Inequalities | Mental health | Policy | Primary, community and social care services | Public health and prevention
Learning from lockdown: support for people experiencing homelessness
There are few clearer measures of societal health than homelessness. On this count, and despite its enormous material wealth, England is in poor shape. Relative to the recent past, and any country we might want to compare ourselves to, we have a problem with homelessness. The causes of homelessness…
 Elective care | Finance and payments | Inequalities
Elective care | Finance and payments | Inequalities
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions. Treatments for these conditions are often expensive: While specialised services support a small proportion of the population, approximately one-sixth of the total NHS budget - over £19 billon - was allocated…
COVID-19: breaking the cycle of deprivation and ill health
Promoting whole-system action on the wider determinants of healthy life expectancy in the shadow of the COVID-19 pandemic
 Elective care | Inequalities | Public health and prevention
Elective care | Inequalities | Public health and prevention
Socio-economic and environmental impact of Herefordshire and Worcestershire STP
Anchor institutions are large, typically non-profit, public sector organisations whose long-term sustainability is tied to the wellbeing of the populations they serve. They also have a significant impact on the health and wellbeing of their local communities. Health and care organisations act as…
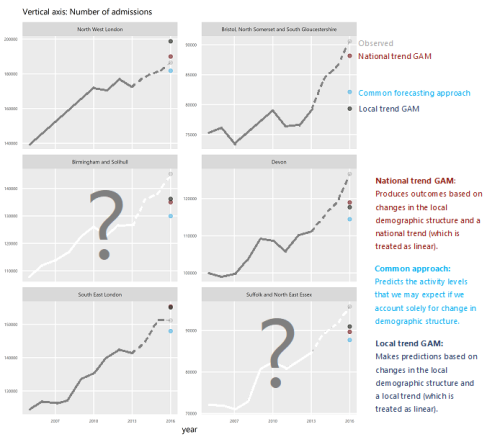
Modelling the impact of covid on waiting lists for planned care
Working with the national collaboration to coordinate covid-related analysis, and the NHSE/I Midlands region, the Strategy Unit has produced a ‘systems dynamics’ model of waiting lists for planned care. The model is freely available for non-commercial use across the NHS. Here, Steven Wyatt and Mike…
How can Integrated Care Systems collect and use more ‘person-centred intelligence’?
Working with our partners Ipsos MORI, we have produced detailed guidance and an offer of services to address this question. This webpage contains information about the work, and all the products from it. Please get in touch if you would like to improve your use of person-…
 Better use of analysis | Inequalities | Public health and prevention
Better use of analysis | Inequalities | Public health and prevention
Midlands Population Health Management Academy
The Midlands Population Health Management Academy was part of a programme of support, commissioned by NHS England and NHS Improvement (Midlands) working in partnership with the Local Government Association and Public Health England. The Programme ran from March 2019 to March 2020. It was designed…
 Elective care | Emergency care | Finance and payments | Policy | Primary, community and social care services
Elective care | Emergency care | Finance and payments | Policy | Primary, community and social care services
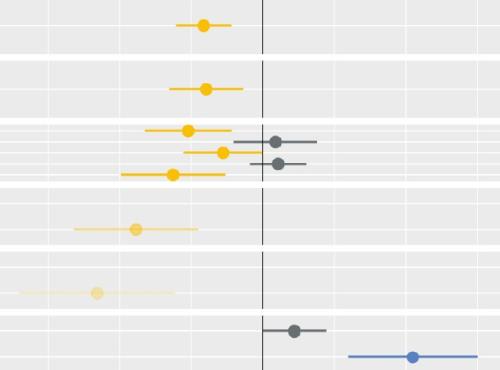
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.