Strategy Unit demand model wins prestigious Florence Nightingale Award
Our open-source demand model, developed in collaboration with the New Hospital Programme, has been named the 2025 winner of the Florence Nightingale Award for Excellence in Health and Care Analytics.
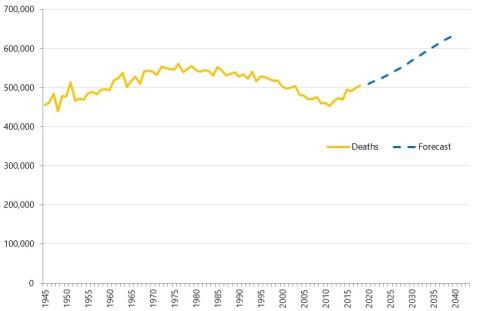
Transforming Hospital Planning with an Open-Source Demand and Capacity Model
We are proud to announce the open-sourcing of a demand and capacity model, developed with the New Hospitals Programme, to transform NHS hospital planning with transparency, collaboration, and efficiency.

Our role in the New Hospital Programme
Learn how the Strategy Unit’s innovative model is transforming hospital planning by providing a consistent, data-driven approach to forecast future demand and evidence-based decision making.

‘Internal Consultancy’: INSIGHTS from evidence and experience
In this blog, our Head of Policy, Fraser Battye, shares his reflections on a recent ‘SU INSIGHTS’ event on the ‘Internal Consultancy’

From ‘right drift’ to ‘left shift’?
Our Head of Policy, Fraser Battye, looks at the challenges facing the intention to shift care ‘from hospital to community’. He suggests that we have missed a critical part of the explanation for why this ‘left shift’ hasn’t taken place following previous initiatives.

Charisma
In this long read, which first appeared in the HSJ, Fraser Battye - our Head of Policy – looks at the role of charisma and innovation in the way that NHS resources are allocated.
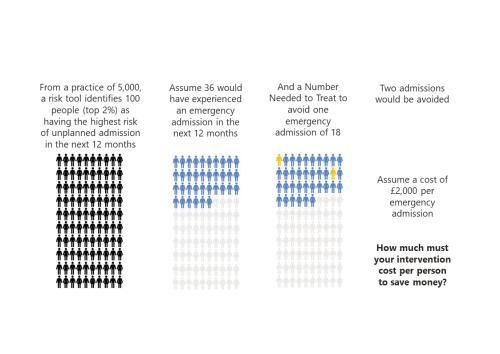
‘To risk stratify or not risk stratify, that is the question’ (At least, it should be)
Risk stratification tools are ubiquitous in healthcare. The concept is simple and seductive.

‘NHS 10 Year Plan’: Strategy Unit consultation response
The Strategy Unit’s response to the Government’s current consultation on the ‘10 Year Health Plan’ for England.

Ara Darzi, Wes Streeting and English health policy. Part 2: cutting the knot
Following on from part one, Fraser continues exploring the Gordian Knot of English health policy.

Ara Darzi, Wes Streeting and English health policy. Part 1: the Gordian Knot
Health policy is not at a crossroads, it is in a bind. Strands so entangled, so complex they resemble a Gordian knot. Can this knot be untied?

The risks of risk stratification
Medical history is full of bizarre and gruesome procedures.

Ghosted by an old friend
“…personal contact was a vital element in general practice from the beginning. By 1959 50% of people in England regarded their GP as a personal friend.”

GP services: new analysis and fresh insights
In our latest analysis for the Midlands Decision Support Network (MDSN), we explore the long standing problem of access to GP practice consultations we consider the implications, and explore potential solutions.

Diagnosing harms?
All medicines are poisons. Everything that cures could kill if administered in the wrong doses, to the wrong people, at the wrong times, in the wrong ways.
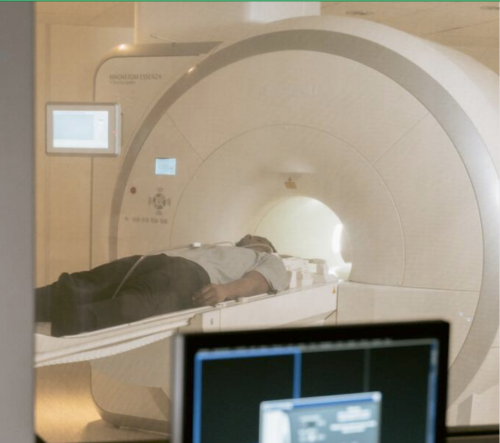
How is growth in diagnostic testing affecting the hospital system?
Diagnostic services, such as medical imaging, endoscopy, and pathology, have grown substantially in recent years and at a faster rate than most other healthcare services. Increased diagnostic testing brings benefits to patients, but rapid growth of this service area within a complex, adaptive system such as the NHS is likely to have had unintended consequences. Midlands ICBs wanted to understand the impact of diagnostic growth on hospital services.
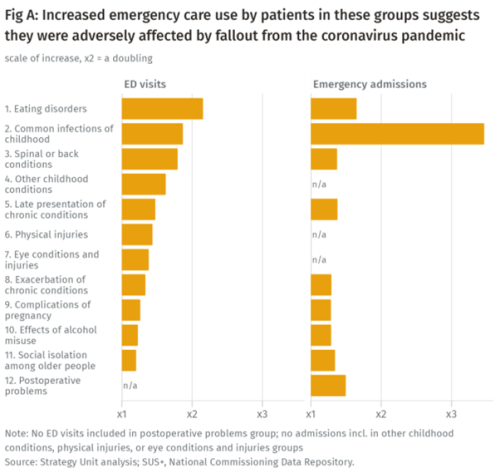
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing inequalities caused by the pandemic.

Infant feeding problems, lockdown and attendance at Emergency Departments: what’s going on?
From our previous work, with Nuffield Trust and Health Foundation, we know that lockdown had a significant effect on attendance at Emergency Departments (ED). We also know that this effect was very unevenly distributed: some demographic groups stayed away far more than others.

The impact of social care on demand for urgent hospital care: have we reached a consensus?
The care home COVID crisis and the effects of longstanding staffing and funding shortages has meant that social care has featured heavily in the media over the last 12 months.
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these experiences can be profound.
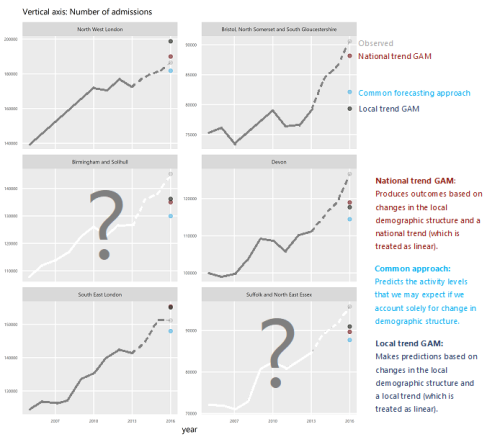
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.