 Better use of analysis | Inequalities | Policy
Better use of analysis | Inequalities | Policy
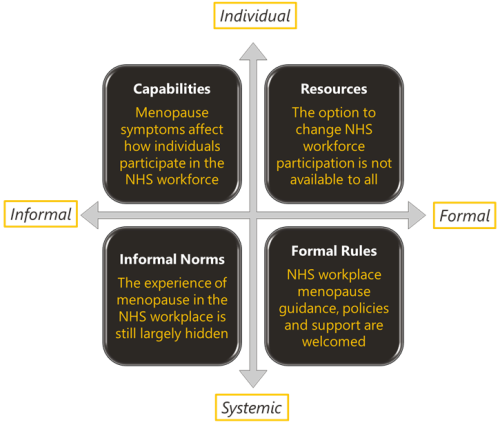
Menopause and the NHS workforce
The impact of the menopause on the NHS workforce. The Strategy Unit and Health Economics Unit report on their mixed methods findings.
 Better use of analysis | Policy | Integrated Care
Better use of analysis | Policy | Integrated Care
ICS intelligence functions – a toolkit to support the implementation of NHSE guidance
In 2020, NHSE announced the expectation that ICSs should develop “shared cross-system intelligence and analytical functions that use information to improve decision-making at every level.” This expectation has been followed by more detailed
 Better use of analysis | Inequalities
Better use of analysis | Inequalities
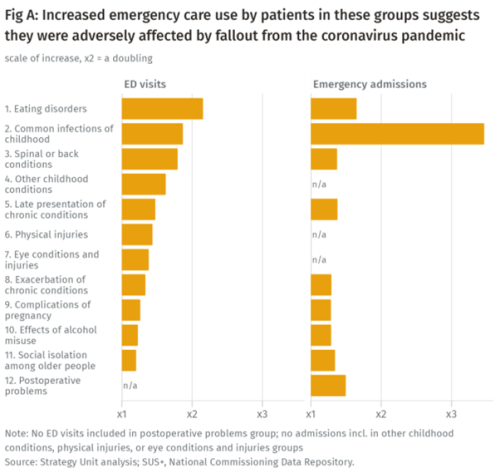
Population health implications of the Covid-19 pandemic
Our new report for The Midlands Decision Support Network (MDSN) presents findings of the effects of the care disruption, from the Covid-19 pandemic, on population health. The in-depth analysis identifies which patients and health conditions should be the focus of future efforts in reducing…
 Mental health | Primary, community and social care services
Mental health | Primary, community and social care services
Inequities in children and young people’s mental health services
Good mental health during early years and childhood has a great bearing on health throughout life. By contrast, poor mental health can cast a long shadow. Consequences may include depression, self-harm, and poor physical health. Services recognise this. They aim to provide access to support in a…
 Better use of analysis | Elective care | Emergency care | Inequalities | Primary, community and social care services | Public health and prevention
Better use of analysis | Elective care | Emergency care | Inequalities | Primary, community and social care services | Public health and prevention
Less noise and more light: using criteria-driven analysis to tackle inequalities
Reducing health inequality is a long-standing aim of health policy. Yet the gap between policy aim and population outcome has grown in recent years: on most measures health inequalities have got worse.
 Elective care | Inequalities | Policy | Primary, community and social care services
Elective care | Inequalities | Policy | Primary, community and social care services
Socio-economic inequalities in access to planned hospital care: causes and consequences
Tacking inequalities in health is a long-standing NHS policy objective. Variation in the experiences and outcomes of different communities during the COVID-19 pandemic served to bring this issue back into focus.
Analytical Collaboration for COVID-19
Between March and December 2020 the Health Foundation; King’s Fund; Nuffield Trust; and the Strategy Unit collaborated to provide analytical support to the health and care system to help in the fight against COVID-19. The organisations worked in a coordinated way to provide…
 Elective care | Finance and payments | Inequalities
Elective care | Finance and payments | Inequalities
Equity and Cost Growth in Specialised Services
NHS specialised services provide care for people with complex or rare medical conditions. Treatments for these conditions are often expensive: While specialised services support a small proportion of the population, approximately one-sixth of the total NHS budget - over £19 billon - was allocated…
 End of life | Inequalities
End of life | Inequalities
Health service use in the last two years of life
Health and care services get just one opportunity to support people at the end of their life. When this support is compassionate and appropriate, unnecessary suffering can be avoided and grieving can be eased. When this is not the case, harm and distress can result. The difference in these…
 Inequalities | Mental health
Inequalities | Mental health
Accessibility of perinatal mental health services for women from Ethnic Minority groups
Barriers to accessing mental health care during pregnancy and the first postnatal year (perinatal period) seem to be greater for ethnic minority women.
 Elective care | Emergency care | Finance and payments | Policy | Primary, community and social care services
Elective care | Emergency care | Finance and payments | Policy | Primary, community and social care services
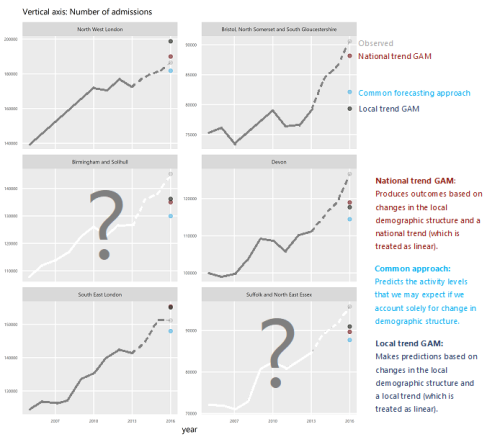
How will we know if Integrated Care Systems reduce demand for urgent care?
The implications of a blended payment system are far reaching: Decisions about planned activity levels will determine the total funding envelope for urgent care within a system and will influence the behaviour of healthcare providers and the services they deliver to patients.
 Elective care | Mental health
Elective care | Mental health
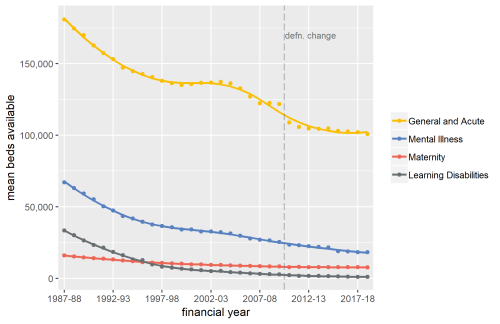
Exploring Mental Health Inpatient Capacity
This report explores the pressures on inpatient mental health services across Sustainability and Transformation Partnerships in England, drawing on a wide range of datasets, published research and interviews with staff working on mental health services. The report was commissioned by and includes…
 Emergency care | Policy
Emergency care | Policy
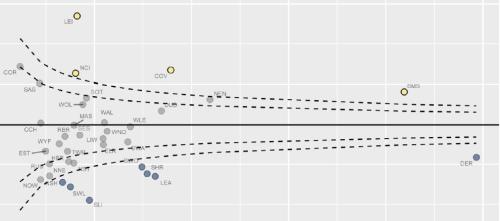
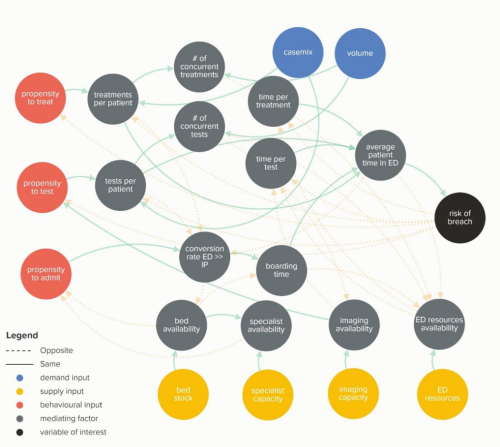
Waiting Times and Attendance Durations at English A&E Departments
In March 2019, NHS England is expected to report the outcome of its review of constitutional waiting times targets. This report reviews the factors that have led to the decline in performance against one of these targets - the 4-hour target for Accident and Emergency Departments. The analysis…
 End of life
End of life
The Status of Electronic Palliative Care Coordination Systems in the West Midlands
Commissioned by NHS England, this report describes the state of electronic palliative care coordination systems in the West Midlands. It draws on a review of the literature, interviews with local NHS staff and responses to information requests. As people approach the end of their lives…
 Inequalities | Mental health
Inequalities | Mental health
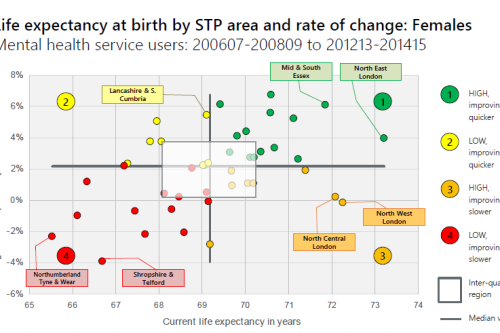
Making the case for integrating physical and mental health services in England - National overview
This is a national overview report of our Making the case for integrating physical and mental health services reporting which took place in July 2017. The original reports looked at the physical health of people who use mental health services; life expectancy, acute hospital use and…
Risk and Reward Sharing for NHS Integrated Care Systems
Risk and reward sharing is a simple and attractive concept, offering a commissioner the opportunity to co-opt and incentivise a provider to moderate growth in healthcare demand by sharing in the savings or cost over-runs. The Centers for Medicare and Medicaid Services (CMS), a US government…
Horizontal or Vertical: Which way to integrate?
In 2011, Primary Care Trusts faced a difficult choice. The Transforming Community Services policy required a complete break of commissioner and provider functions. But what should PCTs do with the community health services they delivered; vertically integrate with an acute trust, horizontally…
 End of life | Inequalities
End of life | Inequalities
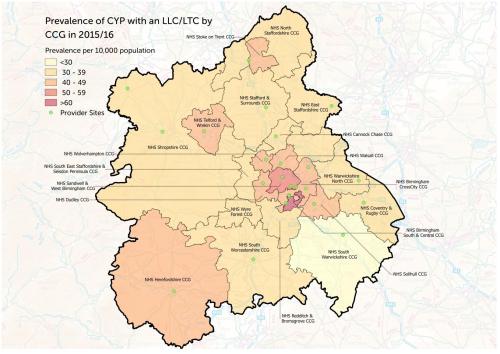
Palliative and End of Life Care Report for Children and Young People
Commissioned by NHS England, this report describes the the characteristics and levels of resource required by children and young people (CYP) (0-25 years) with life limiting conditions and/or life threatening conditions (LLC). The scope of this report does not attempt to explain or address the…
Identifying Potential QIPP Opportunities - Dudley Example
Given the pressures within the NHS, being able to identify opportunities for efficiencies and improvements is vital to inform commissioning intentions. This report is an example of analytical work which to support commissioners. The objective of this report is to provide information to…
 End of life
End of life
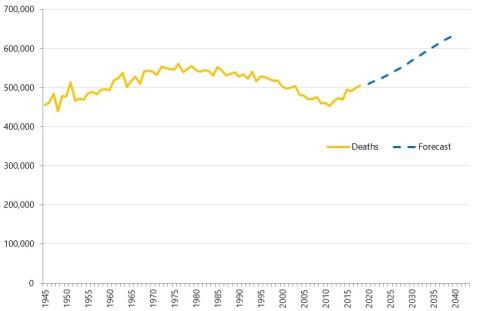
Palliative and End of Life Care in the West Midlands
Commissioned by NHS England, this report describes the status and context of palliative and end of life care services in the six Sustainability and Transformation Partnerships in the West Midlands. The report contains data on trends and forecast numbers of deaths, place of death, palliative…